Clinical & Translational Research, EuroPerio, Treatment, Article
How AI can benefit periodontology and implant dentistry
13 May 2025
Artificial Intelligence is already playing a big role in dentistry and there is much more to come. William Giannobile, professor of oral medicine, infection, and immunity at the Harvard University School of Dental Medicine, reflects on AI in periodontology and implant dentistry and highlights some of the key areas in which clinical practice and research will be impacted.
In broad terms, how is AI going to impact the clinical practice of periodontology and implant dentistry?
Artificial intelligence is going to be (and is already) transformative in healthcare and it has many broad ramifications as it relates to personalized or precision care. One of the very big areas where AI is being leveraged is in biomedical imaging, in radiographic interpretation.
Many AI companies in dentistry are really focused on radiographic imaging and then adding a variety of tools to identify dental caries, periodontal disease, and so on. Looking at bone levels around implants and teeth and then using this concept of computer vision from the radiographs, you can identify a variety of different structures within the oral cavity for those disease states. But you can also identify things like tumours within the jaws and then be able to discriminate different types of tumours. Through machine learning, once these radiographs are annotated, the systems continue to get better and better.
More dental radiographs have been annotated in this way than medical radiographs. And this is where dentistry is leading in the whole field of healthcare, because a patient who goes to the dentist will oftentimes get a full-mouth series of individual radiographs.
There are so many different items on a radiograph that dentists use daily: bone, tooth, implant, soft tissue. We can also see where the root canal is located, if a root canal filling has been done, if there is a certain type of filling or crown or potential pathology. So many things that can be identified and where artificial intelligence can be leveraged. Looking at a radiograph, the naked eye can discriminate, I believe, 64 shares of grey, but it can now be infinite numbers depending on the quality of the AI.
The other big area in dentistry and medicine that is rapidly being improved by AI is pathology. Pathological specimens, histological slides derived from a biopsy, are now being read by AI tools. And this means being able to identify the needle in the haystack in terms of those cancer cells that were maybe somehow missed by a clinician. Or the AI imaging software picks up these different histological or pathological changes and brings them to the attention of the clinician. And it might be something that can be monitored versus something that needs further biopsy, or maybe we're going to have to deliver a specific chemotherapeutic regimen, maybe surgery.
Clinicians might be able refine clinical protocols with this, and it can potentially be used in the development of clinical guidelines. The consensus report of the EFP’s workshop on novel technologies in the diagnosis of periodontal diseases has just been published (see bibliography).
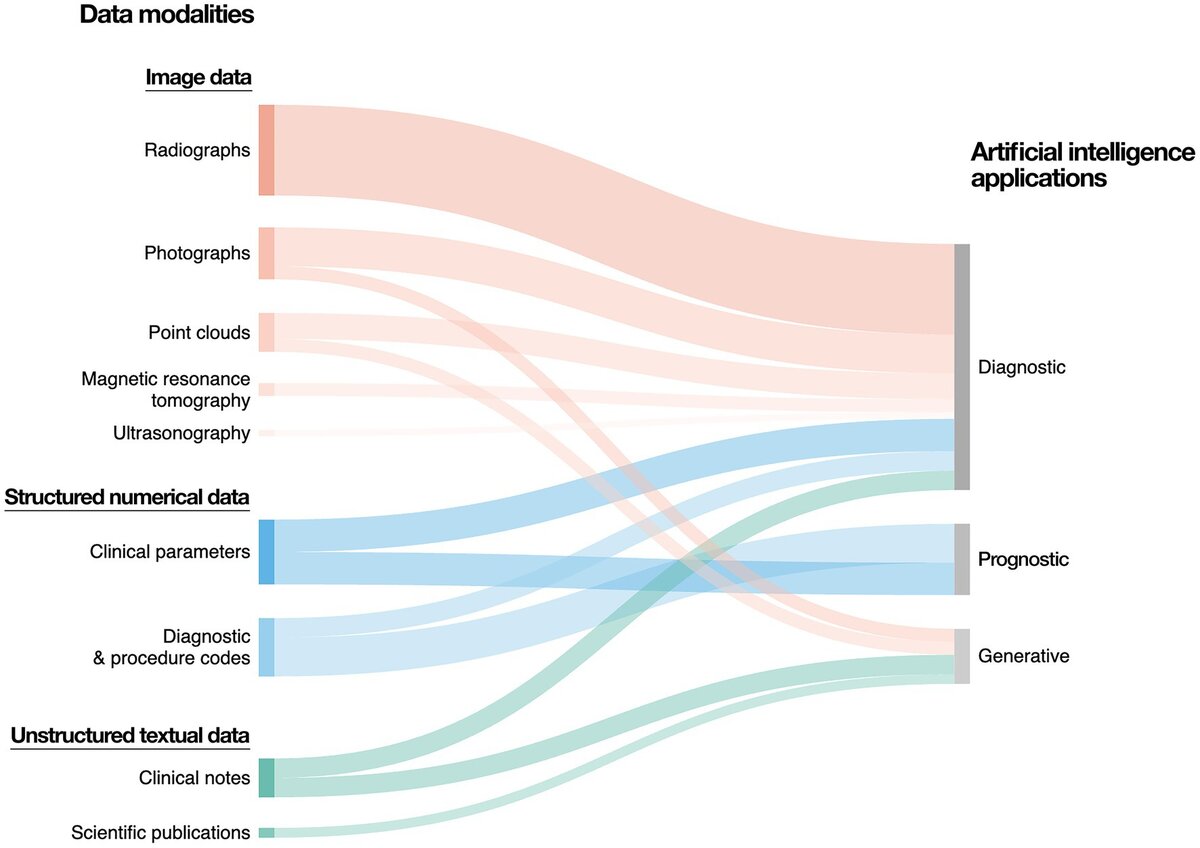
The majority of data generated in dental medicine can be categorized into image data, structured numerical data, as well as unstructured textual data. Image data predominantly includes radiographs, which can be two-dimensional (e.g., panoramic and periapical radiographs, bitewings) or three-dimensional (e.g., computed tomography scans). Further sources of image data include photographs and three-dimensional point clouds (e.g., intraoral scanning). Structured numerical data include demographic data, electronic dental records, as well as clinical parameters (e.g., periodontal probing depth, vertical alveolar bone loss). Unstructured text data include free-form clinical notes, patient testimonials, referrals, treatment plans, as well as academic publications and regulatory documentation.
In what other ways will AI help periodontists in their clinical work?
In terms of the staging and grading of periodontal disease under the 2018 classification, we may be able to be more automated. Diabetes and smoking are part of that grading scheme, and we now have new genetic markers, as we also have different biomarkers of disease. Those can be built into our grading formulas, where we can improve and customize and build off the 2018 guidelines. And this is where AI is going to be able to take it to another level, in my opinion.
How is AI being deployed in terms of research in periodontology and implant dentistry?
We are now seeing AI methods being incorporated into so many different aspects. Back in 2021, we published a study[1] which was the first use of machine learning for risk-stratifying patients who are receiving treatment for peri-implantitis and reconstructive therapy. As a part of that study, we looked not only at the clinical presentation, but also at radiographs, age, all those basic demographics of a patient. We also harvested biopsies from these patients because then they received surgical therapy, laser treatment, bone grafts. And we looked at the immune cells that were comprising those defects around the dental implants. Then we also looked at the microbial composition.
So, what were those bacteria contributing to the disease presence, and then what were the cell populations that were adjacent to that implant? We used research methods to develop a machine-learning algorithm to identify patients who were low risk, moderate risk, and high risk for responding to the intervention.
We’ve also harnessed AI to address oral-health disparities[2], and there’s a recent paper that used some AI models to identify workforce shortages and so-called “dental deserts”[3], really looking at where these patient populations are located.
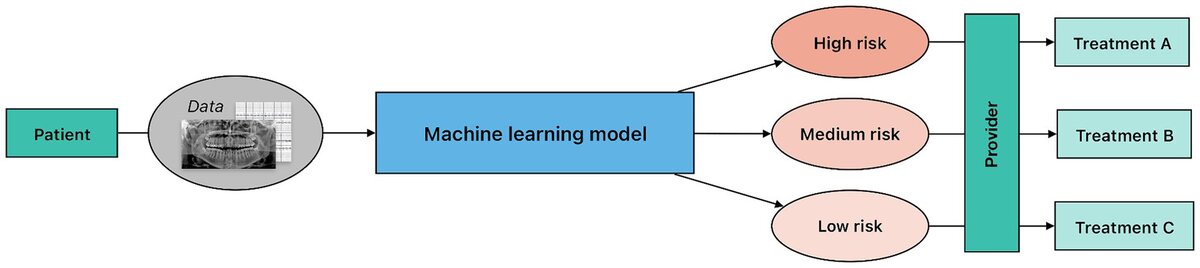
In this process, predictive modelling is applied to patient data to classify individuals into predefined risk categories. Notably, although the underlying machine-learning architecture may be similar to diagnostic modelling, risk stratification predictions lack a definitive ground truth. The provider uses the information from the model to guide the treatment planning and risk prediction at the patient level.
What about the potential problems with AI in terms of replicating cultural biases and in terms of data protection?
From a regulatory standpoint and from a bioethics standpoint, we can see the two big aspects that affect the data. One is you have to examine the variability of any disease, of any specific situation. It could be racial, ethnic, gender differences—all those components will relate to the variance. And so that level of variance is going to be important as these models are developed to look at the individual patient level.
And that builds into bias, which is the other component. Variance and bias. In the models that are being developed, there are conscious and unconscious biases that clinicians may be in putting, indoctrinating into the models.
You hear this when it relates to precision or personalized health. So eventually you may want to incorporate specific attributes at the patient level—for example, female, 40 years old, has cardiovascular diseases, and this is the past medical history. Different rubrics may be developed that can hopefully reduce some of the biases.
Data protection is always a challenge in all of medicine. For example, I did a test with 23andMe (the genomics and biotechnology company that filed for bankruptcy in March this year, raising privacy concerns), and when I took the test, I knew that I was contributing to a data warehouse where they're going to be able to better understand a variety of genetic characteristics associated with disease risk.
In the United States, we have a law for genetic protections—the Genetic Information Non-discrimination Act (GINA)—and we hope we are building trust in many of these systems that they are going to make an appropriate use of the data.
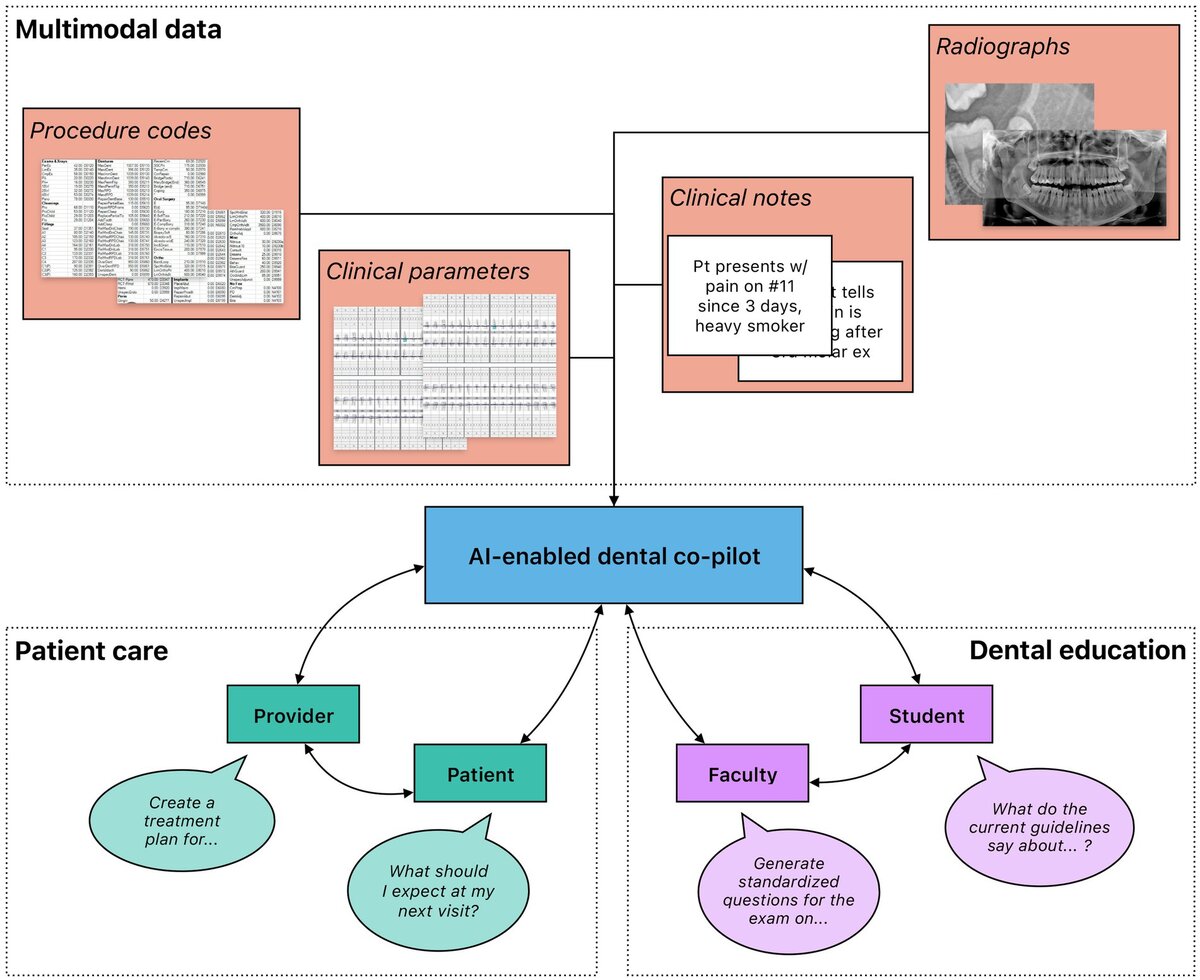
Rich, multimodal data gathered from clinical practice and dental research could be leveraged to train generative AI models that function as co-pilots to dental professionals. These models could be deployed in a variety of different settings, including patient care and dental education. Importantly, multiple stakeholders benefit from their interactions with the models. In patient care, both providers and patients could leverage generative AI to gain information; providers could further automate administrative processes to increase efficiency. In dental education, faculty and students could both engage with generative AI to create an immersive learning environment with individualized feedback.
What about the role of AI in education, whether in terms of university students or at the level of patient education?
Patients are getting engaged and some are using AI to self-diagnose (whereas before they’d ask Dr Google), so they register into a ChatGPT type of software and come in and almost self-diagnose. So, the question for us is how can we, as a dental educator, educate the patients?
AI can become very important with patient compliance because we can customize our care, and it can maybe even affect the recall frequency of the patients. Because some patients are really very low risk, and we can tell those patients maybe they only need to come in once a year. But there are other patients that need to be seen more frequently, and then you can help them become more compliant by telling them, “You’re at risk to lose more teeth and have more of a progressive disease because we have evaluated you in this regard.”
We also need to help our students to use AI as they meet with their faculty members to get some of that background on the literature review, look at some of the likelihood of disease and using AI for that. And then when interviewing the patient, use generative AI with large language models, gathering information to improve clinical care. So, we have AI at the patient side, at the student trainee side, and then at the faculty side. In other words, working together as a team to exert some of those aspects of AI that can help us.
One final message that I want to give is that still clinicians are required in clinical decision-making, and the use of AI is a tool to improve the different diagnostic problem lists that will be assembled in clinical practice, to aid the clinician who can then spend maybe more chair time interacting with the patient.
We are not dealing with a profession that is in danger of being made redundant by AI. However, one of the things that you will probably hear repeated is that dentists who use AI will replace those dentists who don’t use AI.
NOTE: All figures from Feher B, Tussie C and Giannobile WV (2024) Applied artificial intelligence in dentistry: emerging data modalities and modeling approaches. Front. Artif. Intell. 7:1427517. doi: 10.3389/frai.2024.1427517.
[1] Wang CW, Hao Y, Di Gianfilippo R, Sugai J, Li J, Gong W, Kornman KS, Wang HL, Kamada N, Xie Y, Giannobile WV, Lei YL. Machine learning-assisted immune profiling stratifies peri-implantitis patients with unique microbial colonization and clinical outcomes. Theranostics 2021; 11(14):6703-6716. doi:10.7150/thno.57775.
[2] Elani HW, Giannobile WV. Harnessing Artificial Intelligence to Address Oral Health Disparities. JAMA Health Forum. 2024;5(4):e240642. doi:10.1001/jamahealthforum.2024.0642
[3] Rahman MS, Blossom JC, Kawachi I, Tipirneni R, Elani HW. Dental Clinic Deserts in the US: Spatial Accessibility Analysis. JAMA Netw Open. 2024;7(12):e2451625. doi:10.1001/jamanetworkopen.2024.51625
Select bibliography
Wang CW, Hao Y, Di Gianfilippo R, Sugai J, Li J, Gong W, Kornman KS, Wang HL, Kamada N, Xie Y, Giannobile WV, Lei YL. Machine learning-assisted immune profiling stratifies peri-implantitis patients with unique microbial colonization and clinical outcomes. Theranostics 2021; 11(14):6703-6716. doi:10.7150/thno.57775.
Feher B, Tussie C and Giannobile WV (2024) Applied artificial intelligence in dentistry: emerging data modalities and modeling approaches. Front. Artif. Intell. 7:1427517. doi: 10.3389/frai.2024.1427517.
Rahman MS, Blossom JC, Kawachi I, Tipirneni R, Elani HW. Dental Clinic Deserts in the US: Spatial Accessibility Analysis. JAMA Netw Open. 2024;7(12):e2451625. doi:10.1001/jamanetworkopen.2024.51625.
Elani HW, Giannobile WV. Harnessing Artificial Intelligence to Address Oral Health Disparities. JAMA Health Forum. 2024;5(4):e240642. doi:10.1001/jamahealthforum.2024.0642.
Herrera D, Tonetti MS, Chapple I, Kebschull M, Papapanou PN, Sculean A, Abusleme L, Aimetti M, Belibasakis G, Blanco J, Bostanci N, Bouchard P, Buduneli N, Calciolari E, Carra MC, Chackartchi T, Dannewitz B, Danser M, Deng K, Derks J, Dietrich T, Discepoli N, Divaris K, Dommisch H, Donos N, Dutzan N, Eickholz P, Eren Kuru B, Faria Almeida R, Farina R, Feher B, Figuero E, Giannobile W, Gosset, M, Graziani F, Gursoy UK, Hagenfeld D, Jepsen K, Jepsen S, Kumar P, Laine ML, Lambert F, Lang NP, Li Y, Loos B, Madianos P, Matesanz P, Mealey B, Molina A, Montero E, Nibali L, Preshaw P, Rakic M, Ramseier C, Salvi G, Sánchez N, Sanz-Sánchez I, Shapira L, Stavropoulos A, Tamimi F, Teughels W, Tomasi C, Trombelli L, Vassilopoulos S, Verket A, West N, Windisch P, and Sanz M. (2025), Consensus Report of the 20th European Workshop on Periodontology: Contemporary and Emerging Technologies in Periodontal Diagnosis. Journal of Clinical Periodontology. https://doi.org/10.1111/jcpe.14152. Online ahead of print. PMID: 40320757
Giannobile WV, Braun TM, Caplis AK, Doucette-Stamm L, Duff GW, Kornman KS. Patient Stratification for Preventive Care in Dentistry. Journal of Dental Research. 2013;92(8):694-701. doi:10.1177/0022034513492336.
Biography

William Giannobile is Dean and the A. Lee Loomis Professor of Oral Medicine, Infection and Immunity at Harvard University School of Dental Medicine. His continuously NIH-funded research programme over the past 30 years has focused on oral and periodontal regenerative medicine, tissue engineering, and precision medicine. He has produced over 300 manuscripts, textbook chapters, and patents focused on periodontology, regenerative medicine, and oral-health research. He is the editor or co-editor of more than 10 books focused on clinical, translational research, periodontology, and regenerative medicine. Dr Giannobile was the editor-in-chief of the Journal of Dental Research, the official journal of the International Association for Dental Research from 2010-20. His awards include: the Gold Medal for Dental Research and Norton Ross Award for Excellence in Clinical Research from the American Dental Association; the Distinguished Scientist Award from the Academy of Periodontology, International Association for Dental Research; and the EFP International Eminence in Periodontology Award. He is a past president of the American Academy of Periodontology Foundation and of the Osteology Foundation.
Artificial intelligence (AI) in periodontal and implant therapy EuroPerio11 | Vienna | Thursday 15 May, 16.30-18.00
- Magda Feres (moderator; Boston, USA): Introduction
- Nitzan Waisberg (Tel Aviv, Israel): AI as a tool for patient-journey management—present and future
- Maurizio Tonetti (Shanghai, China): Explainable AI in periodontology and implant dentistry—clinical applications
- Bruno Loos (Amsterdam, Netherlands): Big data and AI analyses into the relationships of periodontitis, cardiovascular disease, and diabete
- Discussion
Note: William Giannobile had originally been scheduled to introduce and moderate this session.
EuroPerio11 | Vienna | 14-17 May: Information and Registration




