Clinical & Translational Research, Treatment, Article
How to obtain optimal aesthetic results with tooth-supported restorations to treat terminal dentition in the anterior maxilla
19 January 2026
The treatment of terminal dentition in the anterior maxila is major challenge for clinicians when it comes to obtaining the best aesthetic outcomes. Alberto Fonzar describes how tooth-supported restorations can help in the treatment of stage IV periodontitis.
“Terminal dentition” was traditionally defined in the prosthetic literature as that of patients who are at the transition stage between natural dentition and edentulism (Salvi et al, 1998). More recently, the term has come to be used to define the clinical situation of patients diagnosed with stage IV periodontitis, patients who require a complex, multidisciplinary approach that involves periodontal, implant, and often orthodontic procedures (Mitrani et al, 2025; Sanz et al, 2020). Fixed restorative rehabilitation for such periodontally compromised patients usually includes two options:
- Creating a fixed dental prosthesis by using teeth located in strategically favourable positions as prosthetic abutments.
- Extraction of all the remaining teeth and subsequent implant placement to build a fixed prosthesis supported by implant abutments.
A third option, much less common, consists of the combined use of teeth and implants to suport full-arch dental prostheses.
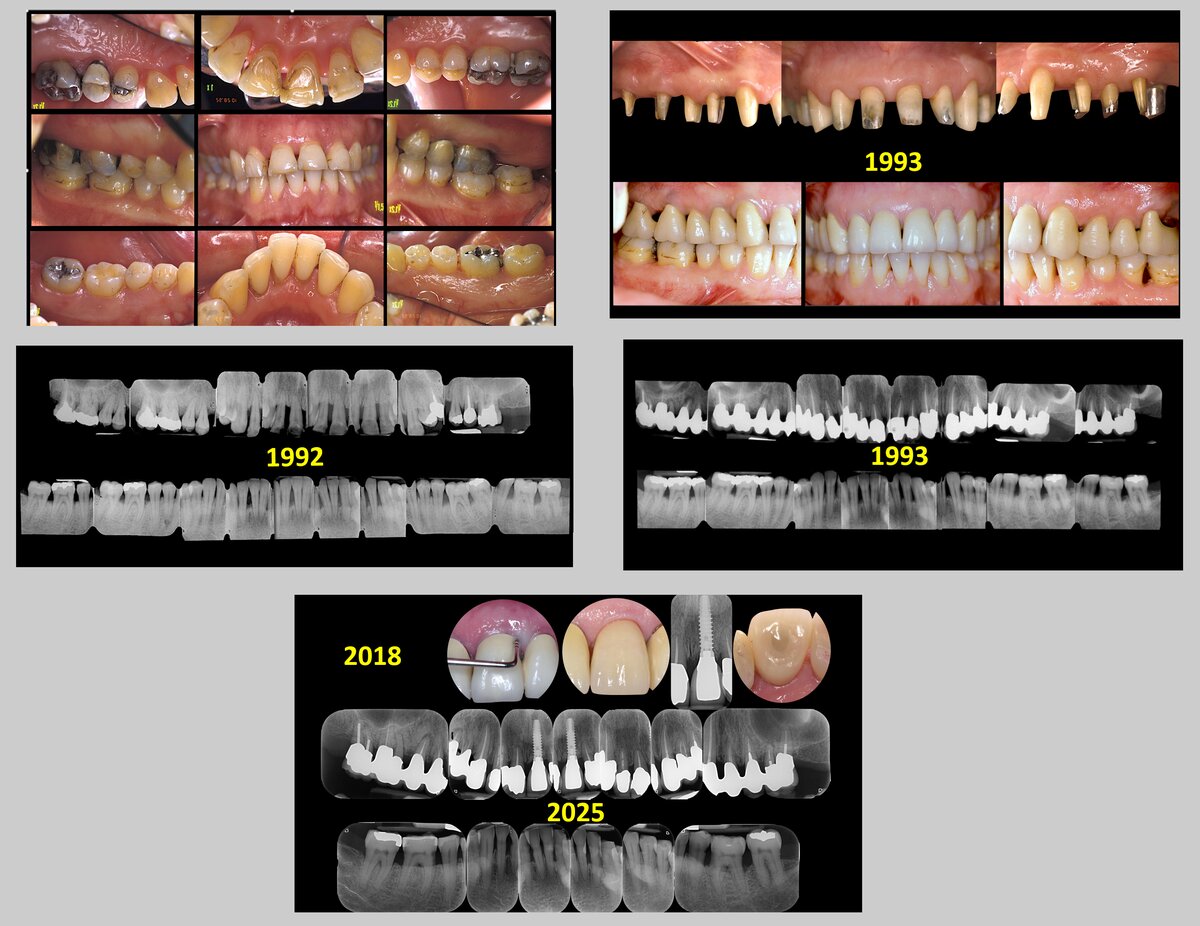
If the goal is to realize a prosthesis with optimal aesthetics, we should first define what we mean by “optimal aesthetics” because the aesthetic perception varies widely from country to country, from person to person, and also between patients and dentists (Tonetti et al, 2025). If we define optimal aesthetics as a smile that appears naturally beautiful and in harmony with the patient’s facial features—so that one should not perceive the difference between restored and natural teeth—we find that this task is extremely difficult to accomplish in patients who have lost five or more teeth and 70-80% of the remaining tooth support (Figure 1). Unfortunately, the only way to achieve “optimal aesthetics” is often to replace the lost tissues with artificial gums. But can this kind of aesthetics be defined as “optimal”?

How do tooth-supported restorations work in stage IV patients?
Sture Nyman and Dan Lundgren in the 1980s and Gianfranco Carnevale and Gianfranco Di Febo in the 1990s demonstrated, with different treatment philosophies, the long-term effectiveness of fixed periodontal-prosthetic treatment. The reliability of these procedures has been confirmed by a systematic review (Montero et al, 2022), which concluded that patients with stage IV periodontitis can be successfully treated with tooth- supported fixed prostheses even in the presence of cantilevers. The recent EFP guidelines on the fixed-prosthetic treatment of stage IV patients recommend the use of a tooth-supported fixed full-arch dental prosthesis both in the maxilla and/or mandible when a sufficient number (four or more abutment teeth) of periodontally maintainable, bilaterally distributed, and restorable teeth is available (Herrera et al, 2022). In a recent systematic review, which compared tooth-supported fixed full-arch dental prosthesis versus implant-supported full-arch prosthesis in stage IV periododontitis patients,the estimated 10-year tooth-abutments loss was lower (1.1%) than the corresponding estimated implant-abutments loss (3.6%) and technical complications were more prevalent at implant-supported restorations compared to tooth-supported ones (Tomasi, 2022).
Tooth-supported restorations in stage IV patients: self-critical analysis
Looking back on my more than 30 years of clinical experience in treating patients with severe periodontitis, I realize that I extracted teeth that could often have been maintained. In other words, I turned into stage IV patients those who were not yet at that stage. This was essentially because I was used to performing a single periodontal re-evaluation at not more than three or four months after the completion of Steps 1 and 2 of periodontal therapy. In other words, neither hard nor soft tissues had had appropriate biologic time to complete the healing process and, as a result, teeth that could have been saved were considered terminal or hopeless. More extractions inevitably lead to more hard- and soft-tissue loss.
For many years now, if the patient’s healing potential seems to have the chance to fully express itself (good self-performed hygiene, not a heavy smoker, no systemic diseases) I do not decide the overall treatment plan at a single periodontal re-evaluation. I wait for the tissue to completely heal. This approach is in line with the EFP clinical guidelines for the treatment of patients with stage IV periodontitis (Sanz et al, 2020; Herrera et al, 2022).
This different approach has significantly reduced the number of teeth judged “terminal” and, consequently, the need to perform a full-arch tooth-supported prosthesis. Patient’s virgin teeth (especially single-rooted teeth in the aesthetic areas) can often be preserved, while in the molar areas occlusion can be provided by implant-supported prostheses.

The consequences of this approach, from both aesthetic and functional perspectives, are substantial. If the goals of periodontal therapy have been achieved (Sanz et al, 2020; Tomasi et al, 2022), the teeth can be orthodontically moved and intruded to compensate for the soft- and hard-tissue loss, and a natural-looking smile is easier to regain (Figure 3). From a functional point of view, the benefit of keeping virgin, and not crowned, teeth is even greater. In teeth that have lost more than 50 per cent of attachment, in order to avoid “black triangles” between the teeth, the prosthetic finishing margin must be located not at the cementoenamel junction but at the gingival margin level, i.e. at the apical third of the root.
Because of the limited thickness of the dentine and the diameter of the dentinal tubules, endodontic treatment is almost inevitable and this dramatically increases the risk of root fracture (Di Febo, 2015). A recent systematic review highlighted that in partially edentulous stage IV patients, teeth used as prosthetic abutments seem to be at greater risk of being lost over time than those not used as abutments, with odds/hazard ratios ranging between 1.7 and 3.2 (Montero et al, 2022).
There are clearly clinical situations in which an implant-supported prosthesis seems to be more appropriate. Tooth-supported restorations are strongly discouraged if the residual tooth support is less than 30 per cent of the root length and in patients susceptible to caries.
Another important limitation of tooth-supported prostheses is related to the type of aesthetics that the patient is looking for. If the patient wishes to achieve a “perfect smile” rather than a natural one, implant-supported prostheses are certainly preferable, as the realization of an artificial gum can compensate for the three-dimensional loss of hard and soft tissues.
The patient’s life expectancy is also a determining factor in deciding between the two options. In a patient with a long life expectancy, I prefer to suggest a tooth-supported prosthesis because, in the worst-case scenario, the use of implants can be postponed for many years.
Finally, the patient's financial resources play a decisive role in choosing between the two options. If no complex procedures are required, the implant option is almost always less expensive, especially if maintaining the teeth requires multidisciplinary procedures.
An important warning: if the patient does not perform an acceptable self-performed oral hygiene, is a heavy smoker, and does not attend the scheduled periodontal supportive therapy, dentures and overdentures are probably the best options.
Lack of scientific evidence
How should we choose between tooth-supported prostheses and implant-supported prostheses in patients with terminal dentition? Unfortunately, we do not have sufficient scientific evidence. Many systematic reviews, especially those related to tooth-supported prostheses, are based on retrospective studies and therefore the data could be influenced by many biases. A recent scoping review on patient preferences between periodontal and implant therapy seems to suggest a strong preference for treatments aimed at preserving teeth, favouring conservative approaches (Gomulinski et al, 2025). When teeth cannot be restored, most patients prefer an implant-supported fixed partial denture to avoid damaging adjacent teeth with a conventional tooth-supported fixed partial denture. But, once again, the evidence is scarce or absent.
To conclude, “terminal dentition” is a term coined by clinicians who ultimately decide the fate of a patient’s remaining teeth based on their personal parameters, clinical experience, and beliefs.
Bibliography
Bevilacqua L, Fonzar A, Olivier S, De Biasi M, Visintin M, Angerame D, Maglione M.Outcome of Different Surgical Approaches in the Treatment of Class II Furcation Defects in Mandibular Molars: A Randomized Clinical Trial. Int J Periodontics Restorative Dent. 2020 Sep/Oct;40(5):693-701.
Cairo F, Nieri M, Cattabriga M, Cortellini P, De Paoli S, De Sanctis M, Fonzar A, Francetti L, Merli M, Rasperini G, Silvestri M, Trombelli L, Zucchelli G, Pini-Prato GP. Root coverage esthetic score after treatment of gingival recession: an interrater agreement multicenter study. J Periodontol. 2010 Dec;81(12):1752-8.
Carnevale G, Fonzar A, Graziani F, Cairo F. The European contribution to osseous resective surgery for the treatment of residual pockets and furcation defects. Periodontol 2000. 2025 Aug 4. doi: 10.1111/prd.70001.
Cortellini P, Tonetti MS, Lang NP, Suvan JE, Zucchelli G, Vangsted T, Silvestri M, Rossi R, McClain P, Fonzar A, Dubravec D, Adriaens P. The simplified papilla preservation flap in the regenerative treatment of deep intrabony defects: clinical outcomes and postoperative morbidity. J Periodontol. 2001 Dec;72(12):1702-12.
Di Febo G, Bedendo A, Romano F, Cairo F, Carnevale G. Fixed prosthodontic treatment outcomes in the long-term management of patients with periodontal disease: a 20-year follow-up report. Int J Prosthodont. 2015 May-Jun;28(3):246-51. doi: 10.11607/ijp.3995. Erratum in: Int J Prosthodont. 2015 Jul-Aug;28(4):424.
Fonzar A. Periodontal prosthesis: control of key factors from surgery to teeth preparation and to final cementation. Int J Esthet Dent. 2014 Summer;9(2):280-96.
Fonzar F, Fonzar A, Buttolo P, Worthington HV, Esposito M. The prognosis of root canal therapy: a 10-year retrospective cohort study on 411 patients with 1175 endodontically treated teeth. Eur J Oral Implantol. 2009 Autumn;2(3):201-8.
Gomulinski S, Gandillot V, Valet F, Agossa K, Huck O, Kerner S, Bouchard P, Carra MC. What Do Patients Prefer in Periodontal and Implant Therapy? A Scoping Review. J Periodontal Res. 2025 Oct;60(10):949-962.
Herrera D, Sanz M, Kebschull M, Jepsen S, Sculean A, Berglundh T, Papapanou PN, Chapple I, Tonetti MS; EFP Workshop Participants and Methodological Consultant. Treatment of stage IV periodontitis: The EFP S3 level clinical practice guideline. J Clin Periodontol. 2022 Jun;49 Suppl 24:4-71.
Lulic M, Brägger U, Lang NP, Zwahlen M, Salvi GE. Ante's (1926) law revisited: a systematic review on survival rates and complications of fixed dental prostheses (FDPs) on severely reduced periodontal tissue support. Clin Oral Implants Res. 2007 Jun;18 Suppl 3:63-72.
Mitrani R, Papaspyridakos P, Bedrossian EA, Goldberg J, Tsigarida A, Chochlidakis K. Treatment planning algorithm for patients with a terminal dentition. J Prosthet Dent. 2025 Nov;134(5):1391-1397.
Montero E, Molina A, Palombo D, Morón B, Pradíes G, Sanz-Sánchez I. Efficacy and risks of tooth-supported prostheses in the treatment of partially edentulous patients with stage IV periodontitis. A systematic review and meta-analysis. J Clin Periodontol. 2022 Jun;49 Suppl 24:182-207.
Nyman S, Ericsson I. The capacity of reduced periodontal tissues to support fixed bridgework. J Clin Periodontol. 1982 Sep;9(5):409-14.
Pilloni A, Montanaro L, Dell'olmo F, Fonzar A, Cairo F, Rojas MA. A retrospective pilot study of correlation of first maxillary premolar root trunk length with age and gender: a cone beam computed tomography study. Minerva Stomatol. 2020 Feb;69(1):27-36.
Salvi GE, Brown CE, Fujihashi K, Kiyono H, Smith FW, Beck JD, Offenbacher S. Inflammatory mediators of the terminal dentition in adult and early onset periodontitis. J Periodontal Res. 1998 May;33(4):212-25.
Sanz M, Herrera D, Kebschull M, Chapple I, Jepsen S, Beglundh T, Sculean A, Tonetti MS; EFP Workshop Participants and Methodological Consultants. Treatment of stage I-III periodontitis-The EFP S3 level clinical practice guideline. J Clin Periodontol. 2020 Jul;47 Suppl 22(Suppl 22):4-60. J Clin Periodontol. 2021 Jan;48(1):163.
Tomasi C, Albouy JP, Schaller D, Navarro RC, Derks J. Efficacy of rehabilitation of stage IV periodontitis patients with full-arch fixed prostheses: Tooth-supported versus Implant-supported-A systematic review. J Clin Periodontol. 2022 Jun;49 Suppl 24:248-271.
Tonetti M, Sanz M, Cairo F, Nart J, Chapple I, Aimetti M, Aroca S, Avila-Ortiz G, Blanco J, Bujaldón A, Cavalcanti R, Cortellini P, Cosyn J, Danser M, de Sanctis M, Derks J, Dommisch H, Figuero E, Gianserra R, Graziani F, Jepsen S, Kebschull M, Lambert F, Montero E, Naenni N, Needleman I, Pilloni A, Ramanauskaite A, Roccuzzo M, Sanz-Martín I, Sanz-Sánchez I, Schwarz F, Sculean A, Stefanini M, Thoma D, Trombelli L, Valles C, West N, Zucchelli G, Zuhr O, Herrera D. Aesthetics and Patient-Reported Outcomes in Periodontology and Implant Dentistry: Consensus Report. J Clin Periodontol. 2025 Sep;52(9):1222-1244.
Tonetti MS, Cortellini P, Lang NP, Suvan JE, Adriaens P, Dubravec D, Fonzar A, Fourmousis I, Rasperini G, Rossi R, Silvestri M, Topoll H, Wallkamm B, Zybutz M. Clinical outcomes following treatment of human intrabony defects with GTR/bone replacement material or access flap alone. A multicenter randomized controlled clinical trial. J Clin Periodontol. 2004 Sep;31(9):770-6.
Tonetti MS, Cortellini P, Suvan JE, Adriaens P, Baldi C, Dubravec D, Fonzar A, Fourmousis I, Magnani C, Muller-Campanile V, Patroni S, Sanz M, Vangsted T, Zabalegui I, Pini Prato G, Lang NP. Generalizability of the added benefits of guided tissue regeneration in the treatment of deep intrabony defects. Evaluation in a multi-center randomized controlled clinical trial. J Periodontol. 1998 Nov;69(11):1183-92.
Tonetti MS, Lang NP, Cortellini P, Suvan JE, Adriaens P, Dubravec D, Fonzar A, Fourmousis I, Mayfield L, Rossi R, Silvestri M, Tiedemann C, Topoll H, Vangsted T, Wallkamm B. Enamel matrix proteins in the regenerative therapy of deep intrabony defects. J Clin Periodontol. 2002 Apr;29(4):317-25.
Biography
Alberto Fonzar graduated cum laude in medicine and surgery at the University of Trieste (Italy) in 1986 and in 1989 earned his specialization in dentistry and prosthodontics at the University of Pisa.Over the last 30 years, Dr Fonzar has specialized in periodontology, implantology, and prosthodontics, becoming one of the top European experts in his field. He is involved in numerous clinical studies and his research has been reported in Italian and international publications. He frequently lectures at congresses and conferences on periodontology and implantology in Europe and the USA. An active member and past president, treasurer, and secretary of SidP (the Italian society of periodontology), Fonzar is also the founder of the International Piezosurgery Academy and an active member of the Italian Academy of Esthetic Dentistry, a visiting professor at the universities of Trieste and Modena, and a member of the Italian Academy of Prosthetic Dentistry and the International College of Dentists.