Systemic health, Article
How do diet and obesity affect periodontitis and the response to treatment?
09 February 2026
There is growing evidence showing that healthy nutrition can play a positive role in preventing periodontal disease while poor diet and obesity can negatively impact both disease and the response to treatment.
James Deschner, Henrik Dommisch, and Johan Wölber consider key issues related to obesity, nutrition, and periodontal disease.
What are the links between obesity and periodontitis?
By James Deschner
Studies showing a link between obesity and periodontitis started almost 50 years ago with a 1977 animal experiment where periodontitis was induced in rats, which showed that the disease became much more severe in the obese rats. It then took around 20 years for clinical studies to confirm this in humans and demonstrate an association between periodontitis and obesity.
Later studies have shown that the relationship is dose dependent: the higher the body mass index (BMI), the higher the risk of periodontitis. This much is clear.
Some studies have also shown that obesity may compromise the outcomes of periodontitis treatment, but other studies have not been able to confirm this and more research is needed.
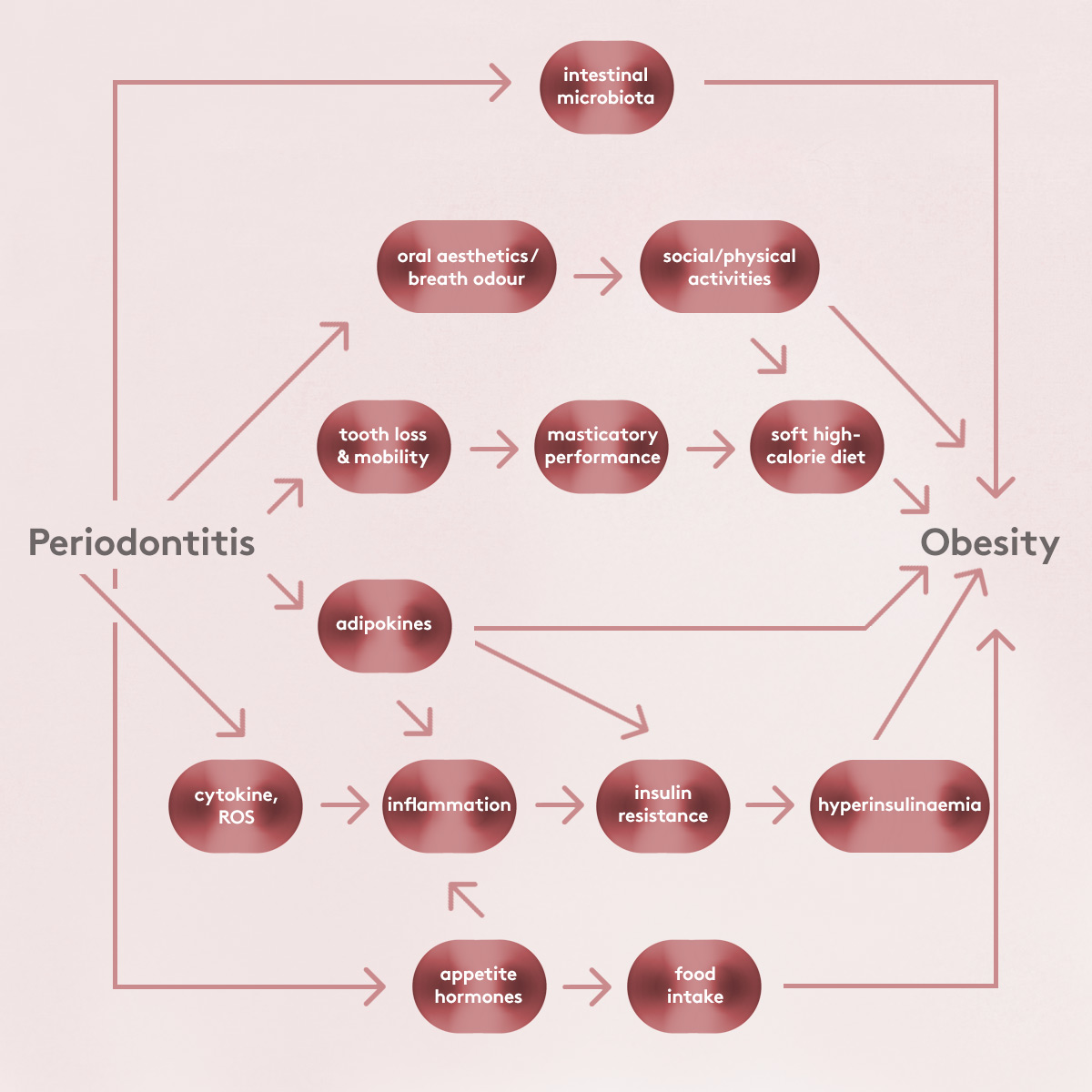
We do not yet fully understand all the mechanisms underlying the association between obesity and periodontitis. One mechanism that may well be involved is that bacteria-induced local periodontal inflammation gets enhanced by the chronic low-grade systemic inflammation induced by obesity. Other possible mechanisms include:
- Obesity produces hyposalivation, which may promote plaque accumulation.
- Obesity might compromise the microcirculation in the gingiva.
- It is also believed that the intestinal microbiome is linked to the oral microbiome. The intestinal microbiome is not only partly responsible for the risk of obesity but can also cause the intestinal barrier to become more permeable, allowing bacterial toxins to enter the systemic blood circulation, which in turn can further increase inflammation locally in the periodontium. In addition, changes in the intestinal barrier can negatively affect the immune system, which is also critical for controlling and combating oral pathogens.
Although the link between obesity and periodontitis is clear and these mechanisms may help to explain it, further studies are needed to clarify the causality—i.e., whether obesity contributes to the development and progression of periodontitis or, conversely, whether periodontitis promotes weight gain. In contrast, causality in the relationship between periodontitis and diabetes is much better understood and proven.
There are reasons to think that periodontitis—particularly in its more severe form (stages III and IV)—may contribute, albeit indirectly, to obesity. If someone is suffering from edentulism or tooth mobility, they may be more likely to opt for a calorie-rich soft diet.
While obesity is clearly a risk modifier, it may well be a true risk factor. We know that, irrespective of periodontitis, obesity causes a pro-inflammatory state and that the inflammation induced by obesity affects the host response, how cells sense microorganisms, and whether the host cells fight against these microorganisms. We also know that obesity affects extracellular matrix molecules of the periodontium. Putting all this together suggests that obesity is a true risk factor for periodontal disease.
There are also shared risk factors: age, alcohol consumption, low socioeconomic level, and low health awareness may contribute to the development of both obesity and periodontitis.
How does nutrition affect periodontal status?
By Henrik Dommisch
Dietary habits and body weight are very much related to each other and there is now a body of evidence showing that eating certain nutritional elements—such as fibres, fruits, and vegetables—is very much related to a better periodontal status, while a very high intake of processed foods and sugar is linked to a more unfavourable status.
We have studies—mostly surveys but also some interventional studies—that give us some hints about the impact of nutritional factors on periodontal status. There are studies showing changes in both the gut and the oral microbiomes, and we have some evidence from studies of fasting, showing what happens to periodontal health if you abstain from sugar for a certain period.
What we find from large-scale studies is that there is a direct relationship between nutritional factors such as a high intake of saturated fats, trans fats, and sugar and periodontal inflammation.
One important question is whether the positive effects that we see in terms of specific dietary regimes result from the diets themselves or from the reduction in body weight.
We do know that diet has a direct influence on the microbiome. In the oral microbiome, processed carbohydrates such as free sugars get transformed or metabolised as short-chain carboxyl acids, which are very pro-inflammatory. We also know that diet can have a direct influence on the dental biofilm.
Some studies have provided evidence that changing the dietary intake could influence periodontal inflammation. However, other studies have not shown such an influence.
There are also studies showing that changes in nutrition caused measurable alterations in the periodontium. For instance, a change to the Mediterranean diet or intermittent fasting or fasting can improve factors such as bleeding on probing.
An increased fibre intake and the adoption of a vegetable-based or vegan diet may lead not only to a clear change in the composition of the gut microbiome but also have some effects in the oral microbiome. Thus, dietary changes may influence the inflammatory status in the oral cavity.
What is the best diet for periodontal health?
By Johan Wölber
While there are differences in dietary guidelines between different countries, there are some things we can all agree on, such as reducing the free-sugar intake—we have a clear meta-analysis and systematic review showing that reducing free sugars will also help to reduce gingival inflammation (Woelber et al., 2023).
Beyond that, choosing a specific diet is a complex issue in terms of individual patients. We have patients who love to eat sausages and those who love to eat pasta, and we have to think about how we can individually motivate patients to make even slight changes in their diet towards a healthier lifestyle.
One way to look at diet is in terms of a daily risk factor, as three times a day most people can make a choice between pro- or anti-inflammatory foods. Periodontists can help here by making their patients aware of this choice and giving them knowledge of the components of an anti-inflammatory diet.
We can agree on increasing the intake of fruit and vegetables, getting sufficient omega-3 fatty acids (maybe two portions of seafood a week), and reducing the intake of processed carbohydrates (such as sugar, white flour, and sugar-sweetened beverages), meat and red meat. There is no need to necessarily become vegan or vegetarian, but most observational data shows that it is generally beneficial for the body to have a reduced intake of saturated fatty acids and red and processed meats. There may also be benefits from intermittent fasting.
In terms of micronutrients, we need to ensure we get enough vitamin D in the winter and other micronutrients such as vitamins A, B, C, and E and phytonutrients.
Most of the intervention studies we have relate to gingivitis—i.e., periodontal inflammation—rather than periodontitis, because it takes much longer to investigate periodontal effects or periodontal outcomes. Nonetheless, we do see clear effects on the bleeding-on-probing score and other relevant clinical factors. This means that a patient really has nothing to lose by trying these dietary changes (other than perhaps losing some excess weight).
There is a need for future research to investigate more thoroughly the potential positive influence from diet and weight reduction on periodontal outcomes and periodontal therapy.

Bibliography
Akram Z, Safii SH, Vaithilingam RD, Baharuddin NA, Javed F, Vohra F. Efficacy of non-surgical periodontal therapy in the management of chronic periodontitis among obese and non-obese patients: a systematic review and meta-analysis. Clin Oral Investig. 2016 Jun;20(5):903-14. doi: 10.1007/s00784-016-1793-4. Epub 2016 Mar 23. PMID: 27005812.
Bartha V, Exner L, Schweikert D, Woelber JP, Vach K, Meyer AL, Basrai M, Bischoff SC, Meller C, Wolff D. Effect of the Mediterranean diet on gingivitis: A randomized controlled trial. J Clin Periodontol. 2022 Feb;49(2):111-122. doi: 10.1111/jcpe.13576. Epub 2021 Dec 5. PMID: 34818686.
Cores Ziskoven P, Nogueira AVB, Yoldaş O, Buduneli N, Wild PS, Koeck T, Deschner J. Apelin – A New Kid on the Block in Periodontology. Oral Health Prev Dent. 2024 Aug 27;22:417-424. doi: 10.3290/j.ohpd.b5695264. PMID: 39189510; PMCID: PMC11619819.
Deschner J, Eick S, Damanaki A, Nokhbehsaim M. The role of adipokines in periodontal infection and healing. Mol Oral Microbiol. 2014 Dec;29(6):258-69. doi: 10.1111/omi.12070. Epub 2014 Sep 27. PMID: 25052571.
Dommisch H, Kuzmanova D, Jönsson D, Grant M, Chapple I. Effect of micronutrient malnutrition on periodontal disease and periodontal therapy. Periodontol 2000. 2018 Oct;78(1):129-153. doi: 10.1111/prd.12233. PMID: 30198127.
Gerber FA, Sahrmann P, Schmidlin OA, Heumann C, Beer JH, Schmidlin PR. Influence of obesity on the outcome of non-surgical periodontal therapy - a systematic review. BMC Oral Health. 2016 Sep 2;16(1):90. doi: 10.1186/s12903-016-0272-2. PMID: 27590050; PMCID: PMC5010690.
Gorman A, Kaye EK, Apovian C, Fung TT, Nunn M, Garcia RI. Overweight and obesity predict time to periodontal disease progression in men. J Clin Periodontol. 2012 Feb;39(2):107-14. doi: 10.1111/j.1600-051X.2011.01824.x. Epub 2011 Dec 12. PMID: 22150475; PMCID: PMC3258330.
Jepsen S, Suvan J, Deschner J. The association of periodontal diseases with metabolic syndrome and obesity. Periodontol 2000. 2020 Jun;83(1):125-153. doi: 10.1111/prd.12326. PMID: 32385882.
Mao JS, Cui HY, Zhou XZ, Zhang SW. Recent Progress in Exploring Dietary Nutrition and Dietary Patterns in Periodontitis with a Focus on SCFAs. Nutrients. 2025 Oct 2;17(19):3150. doi: 10.3390/nu17193150. PMID: 41097227; PMCID: PMC12526378.
Morita I, Okamoto Y, Yoshii S, Nakagaki H, Mizuno K, Sheiham A, Sabbah W. Five-year incidence of periodontal disease is related to body mass index. J Dent Res. 2011 Feb;90(2):199-202. doi: 10.1177/0022034510382548. PMID: 21270462.
Nascimento GG, Leite FR, Conceição DA, Ferrúa CP, Singh A, Demarco FF. Is there a relationship between obesity and tooth loss and edentulism? A systematic review and meta-analysis. Obes Rev. 2016 Jul;17(7):587-98. doi: 10.1111/obr.12418. Epub 2016 Apr 29. PMID: 27125768.
Nishida N, Tanaka M, Hayashi N, Nagata H, Takeshita T, Nakayama K, Morimoto K, Shizukuishi S. Determination of smoking and obesity as periodontitis risks using the classification and regression tree method. J Periodontol. 2005 Jun;76(6):923-8. doi: 10.1902/jop.2005.76.6.923. PMID: 15948686.
Papageorgiou SN, Reichert C, Jäger A, Deschner J. Effect of overweight/obesity on response to periodontal treatment: systematic review and a meta-analysis. J Clin Periodontol. 2015 Mar;42(3):247-61. doi: 10.1111/jcpe.12365. Epub 2015 Feb 20. PMID: 25580635.
Pappe CL, Kleine Bardenhorst S, Prior K, Steckhan N, Michalsen A, Ehmke B, Dommisch H, Hagenfeld D. Impact of Prolonged Fasting on the Oral Microbiome in Patients With Metabolic Syndrome: An Exploratory Secondary Analysis. J Clin Periodontol. 2025 Aug;52(8):1125-1135. doi: 10.1111/jcpe.14171. Epub 2025 May 12. PMID: 40356261; PMCID: PMC12259404.
Pappe CL, Lutzenberger S, Goebler K, Meier S, Jeitler M, Michalsen A, Dommisch H. Effect of a Whole-Food Plant-Based Diet on Periodontal Parameters in Patients With Cardiovascular Risk Factors: A Secondary Sub-Analysis of a Randomized Clinical Trial. J Clin Periodontol. 2025 Jan;52(1):125-136. doi: 10.1111/jcpe.14066. Epub 2024 Oct 14. PMID: 39402877; PMCID: PMC11671171.
Pappe CL, Maetschker J, Dujardin S, Peters B, Pivovarova-Ramich O, Kandil F, Michalsen A, Breinlinger C, Steckhan N, Koppold D, Dommisch H. Intermittent Fasting Regimes Reduce Gingival Inflammation: A Three-Arm Clinical Trial. J Clin Periodontol. 2025 May;52(5):681-694. doi: 10.1111/jcpe.14151. Epub 2025 Mar 9. PMID: 40059409; PMCID: PMC12003054.
Pappe CL, Peters B, Pivovarova-Ramich O, Schremmer R, Adam A, Vach K, Dommisch H, Woelber JP. Effects of a 4-week free-sugar avoidance during periodontal therapy: An explorative randomized controlled clinical trial. J Periodontol. 2025 Jun;96(6):675-690. doi: 10.1002/JPER.24-0208. Epub 2024 Aug 26. PMID: 39185702; PMCID: PMC12273752.
Pappe CL, Steckhan N, Hoedke D, Jepsen S, Rauch G, Keller T, Michalsen A, Dommisch H. Prolonged multimodal fasting modulates periodontal inflammation in female patients with metabolic syndrome: A prospective cohort study. J Clin Periodontol. 2021 Apr;48(4):492-502. doi: 10.1111/jcpe.13419. Epub 2021 Feb 2. PMID: 33393121.
Perlstein MI, Bissada NF. Influence of obesity and hypertension on the severity of periodontitis in rats. Oral Surg Oral Med Oral Pathol. 1977 May;43(5):707-19. doi: 10.1016/0030-4220(77)90055-x. PMID: 266151.
Saito T, Shimazaki Y, Koga T, Tsuzuki M, Ohshima A. Relationship between upper body obesity and periodontitis. J Dent Res. 2001 Jul;80(7):1631-6. doi: 10.1177/00220345010800070701. PMID: 11597023.
Saito T, Shimazaki Y, Sakamoto M. Obesity and periodontitis. N Engl J Med. 1998 Aug 13;339(7):482-3. doi: 10.1056/NEJM199808133390717. PMID: 9705695.
Suvan J, D'Aiuto F, Moles DR, Petrie A, Donos N. Association between overweight/obesity and periodontitis in adults. A systematic review. Obes Rev. 2011 May;12(5):e381-404. doi: 10.1111/j.1467-789X.2010.00808.x. Epub 2011 Feb 23. PMID: 21348914.
Van Ravensteijn MM, Timmerman MF, Brouwer EAG, Slot DE. The effect of omega-3 fatty acids on active periodontal therapy: A systematic review and meta-analysis. J Clin Periodontol. 2022 Oct;49(10):1024-1037. doi: 10.1111/jcpe.13680. Epub 2022 Jul 21. PMID: 35713248; PMCID: PMC9795982.
Woelber JP, Al-Ahmad A, Alt KW. On the Pathogenicity of the Oral Biofilm: A Critical Review from a Biological, Evolutionary, and Nutritional Point of View. Nutrients. 2022 May 23;14(10):2174. doi: 10.3390/nu14102174. PMID: 35631315; PMCID: PMC9144701.
Woelber JP, Gärtner M, Breuninger L, Anderson A, König D, Hellwig E, Al-Ahmad A, Vach K, Dötsch A, Ratka-Krüger P, Tennert C. The influence of an anti-inflammatory diet on gingivitis. A randomized controlled trial. J Clin Periodontol. 2019 Apr;46(4):481-490. doi: 10.1111/jcpe.13094. Epub 2019 Apr 2. PMID: 30941800.
Woelber JP, Gebhardt D, Hujoel PP. Free sugars and gingival inflammation: A systematic review and meta-analysis. J Clin Periodontol. 2023 Sep;50(9):1188-1201. doi: 10.1111/jcpe.13831. Epub 2023 May 28. PMID: 37246336.
Wright DM, McKenna G, Nugent A, Winning L, Linden GJ, Woodside JV. Association between diet and periodontitis: a cross-sectional study of 10,000 NHANES participants. Am J Clin Nutr. 2020 Dec 10;112(6):1485-1491. doi: 10.1093/ajcn/nqaa266. PMID: 33096553.
Biographies

James Deschner is chair of the EFP’s scientific affairs committee and professor and director of the University Medical Center of Johannes Gutenberg University in Mainz, Germany. His research focuses on translational and basic science in periodontal inflammation, immunology, and regeneration. His work also explores interactions between periodontitis and systemic diseases, especially obesity, diabetes mellitus, and metabolic syndrome. Professor Deschner has held prestigious academic appointments worldwide, including research stays and visiting professorships across different continents.
Henrik Dommisch is professsor and chair of periodontology, oral medicine, and oral surgery at Charité – University Medicine Berlin, a former president of the German Society of Periodontology and the current president of the Berlin Society of Periodontology. His research focuses on innate immune responses, the influence of fasting on periodontal inflammation, targeted therapy, drug delivery systems in the treatment of oral inflammatory diseases, genetic risk factors for periodontal diseases, the treatment of endo-perio lesions, and resective and regenerative periodontal therapy.
Johan Wölber is a professor of periodontology and head of the department of periodontology at the Carl Gustav Carus Medical Faculty at TU Dresden. He received his academic and clinical training at the University Medical Center Freiburg, where he spent more than 15 years in clinical practice, research, and teaching, and completed his doctorate in dentistry. His work has been recognized with several national and international awards for excellence in dental education and research. In addition to periodontology, his expertise includes the relationship between nutrition and oral health.




