Public health & Prevention, Systemic health, Article
How periodontal diseases affect women’s health at different stages of life
27 October 2025
Periodontitis affects women differently from men, most notably at times of hormonal changes such as puberty, pregnancy, and the menopause. There is also evidence of an association between periodontitis and breast cancer. James Deschner (chair of the EFP scientific affairs committee) and Lisa Hezel (member of the EFP communications committee) explain the key areas of women’s health in relation to periodontal and oral health.
What are the key areas of women's health that are related to periodontal health?
Women's health and periodontal health are closely linked in several areas. Hormonal fluctuations, particularly those involving oestrogen and progesterone, play a significant role in these connections throughout a woman's life.
For instance, gingival inflammation can occur during puberty because of increased hormonal activity. Similarly, in some women the menstrual cycle can promote cyclical gingival inflammation.
The use of oral contraceptives—especially older, high-dose versions—has also been associated with gingival inflammation, though modern low-dose contraceptives tend to have a lesser effect on gingival health.
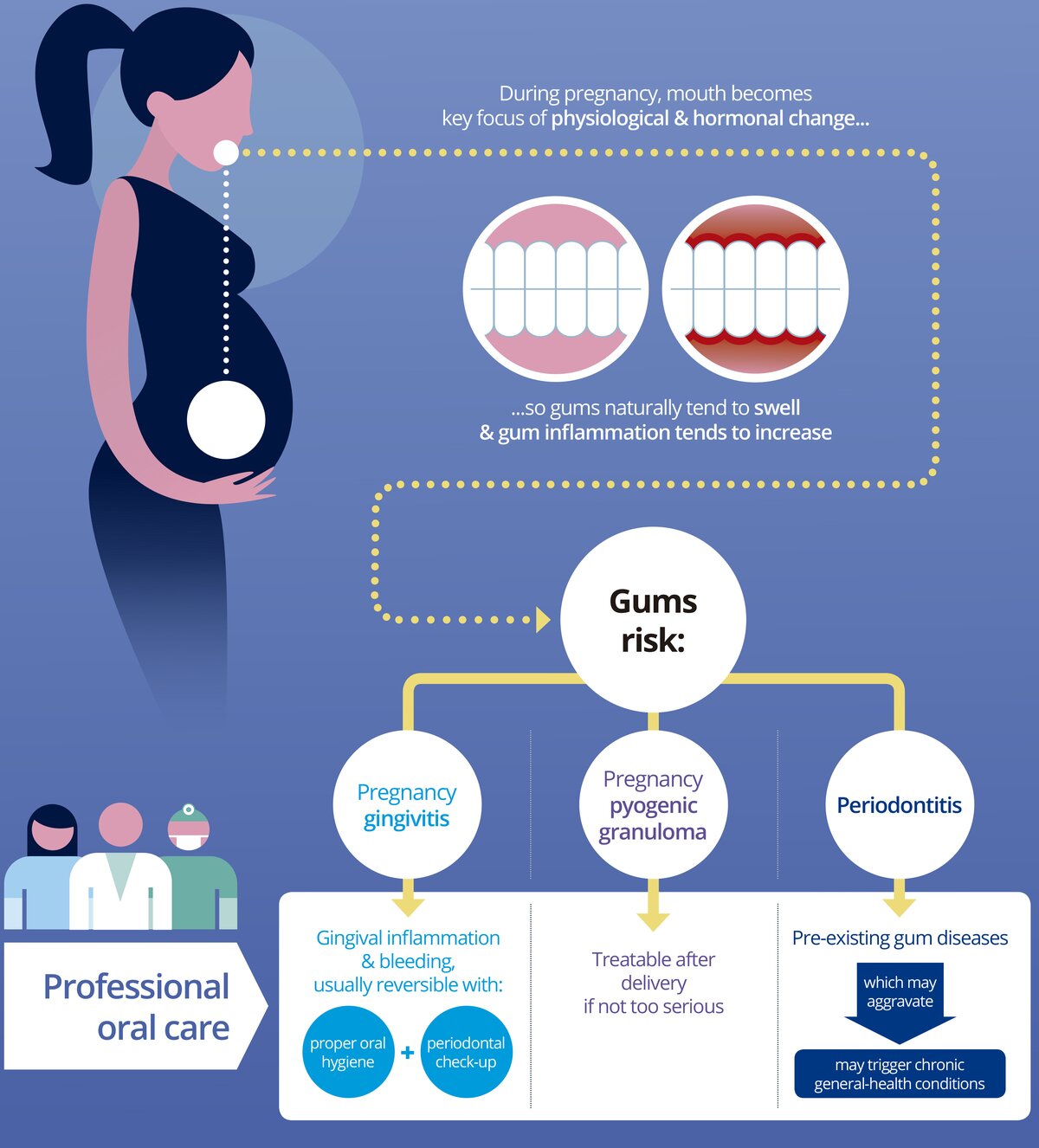
During pregnancy, hormonal changes can exacerbate gingival inflammation and, in some cases, pyogenic granulomas—non-cancerous tumours—can form on the gingiva.
Furthermore, periodontitis during pregnancy is associated with several conditions and complications: an increased risk of preterm birth and low birth weight, pre-eclampsia (a pregnancy-related condition characterized by high blood pressure), and gestational diabetes.
Women with periodontitis are more likely to suffer from polycystic ovary syndrome and possibly endometriosis. It has therefore been suggested that poor oral/periodontal health may be a factor that favours female infertility.
In menopause, a reduction in oestrogen levels is associated with several oral-health concerns—including xerostomia (dry mouth) and burning-mouth syndrome—and an increased risk of osteoporosis, which in turn is linked to a higher risk of periodontal diseases and tooth loss.
Pregnancy is clearly a key moment. What are the pregnancy risks related to periodontal disease and what steps should a pregnant woman take in terms of her periodontal health? At what moments during pregnancy is it appropriate to receive treatment?
Hormonal fluctuations during pregnancy, particularly increases in progesterone and oestrogen, can increase blood flow to the gingiva and make it more susceptible to inflammation. Studies have also demonstrated an association between periodontitis and several adverse pregnancy outcomes, including gestational diabetes, pre-eclampsia, premature birth, and low birth weight.
Intervention studies conducted during the second trimester have attempted to clarify whether periodontitis increases the risk of these pregnancy complications. Some studies have indicated that treating periodontitis may reduce the incidence of premature births and low birth weight in newborns. But other studies have failed to show this positive effect. To date, meta-analyses have been unable to conclusively show whether periodontal treatment can reduce the risk of preterm birth or low birth weight. However, at least two recently published meta-analyses do suggest that the risk may be indeed reduced by certain periodontal treatment strategies (Salama et al., 2024; Wu et al., 2024).
Overall, while periodontitis is clearly associated with premature births and low birth weight, whether this relationship is causal still needs to be investigated further. The debate continues over whether common risk factors such as smoking could be responsible for the observed correlation.
It is also possible that periodontal intervention in the second trimester may be too late to significantly alter the course of pregnancy. Nevertheless, numerous intervention studies have confirmed that periodontal treatment in the second trimester is safe for both the mother and the unborn child. In most cases, non-surgical treatment is performed if the patient accepts periodontal treatment during pregnancy.
How do the menopause and hormone-replacement therapy affect women's periodontal health?
Menopause and hormone-replacement therapy both have a significant impact on women's periodontal health, mainly because of the changes in hormone levels that occur during this time. During menopause, there is a decrease in oestrogen levels in the body, which can have various effects on oral health. For example, oestrogen deficiency can reduce saliva production and lead to xerostomia, which can increase the risk of caries, gingivitis, and periodontitis.
Oestrogen has anti-inflammatory effects, inhibits bone resorption, and promotes bone formation, which means that oestrogen deficiency can lead to net bone loss, with a deterioration of both bone density and bone microarchitecture. Women are therefore significantly more likely than men to suffer from osteoporosis, which also requires treatment. It should be noted here that antiresorptive and bone anabolic drugs are often used in the treatment of osteoporosis. Although these drugs are associated with a risk of drug-associated jaw necrosis, this risk is relatively low in the treatment of postmenopausal osteoporosis.
Hormone-replacement therapy is often prescribed to alleviate menopausal symptoms by restoring oestrogen levels. Its effects on periodontal health can be beneficial or neutral, depending on individual health factors and the specific therapy. Some studies suggest that oestrogen therapy may have a protective effect on periodontal tissues by reducing inflammation and potentially improving gingival health. Oestrogen may promote collagen production and bone metabolism. But not all studies agree on the benefits of hormone-replacement therapy for periodontal health, and although it may have some benefits, its effectiveness seems to vary and needs to be considered on an individual basis.
What is the latest research on how women’s health affects the health of their children?
Women's health is, of course, closely linked to the health of their offspring, and this may also apply to matters of periodontal health. Two interesting studies on this topic were recently published. One noteworthy study examined the subgingival proteome and microbiome of mothers with periodontal disease and their offspring, and it showed that the maternal periodontal microbiome and proteome are associated with those of the offspring and are also related to the maternal periodontal status. This could promote the susceptibility of offspring to dysbiosis and predispose them to periodontitis (Paz et al., 2025).
Another study focused on the microbial colonization in different dentition phases in individuals from birth to 18 years who either came from families with a history of periodontitis or from periodontally healthy parents. It was also found that the periodontal status of parents significantly influences the composition of their children's microbiome from an early age. Moreover, it was found that the mixed-dentition period was the phase associated with establishing a dysbiotic and pathogen-rich microbiome in offspring of parents with periodontitis (Reis et al., 2023). During the mixed-dentition phase, biofilm is difficult to control. The accumulation of dental plaque can be exacerbated during this phase by the eruption of permanent teeth and by parents paying less attention to their children's tooth-brushing. In the children of parents with periodontal disease, transmitted pathogens could exploit this phase of instability to establish themselves permanently in the mouth.
It is well known that diabetes mellitus is associated with periodontitis. Does this also apply to gestational diabetes?
Yes. There is a significant association between periodontal disease and gestational diabetes. Periodontitis could promote the development of gestational diabetes by increasing the insulin resistance. Conversely, impaired glucose metabolism promotes the development or worsening of periodontal diseases.
Periodontitis is also associated with an increased risk of cancer. Is breast cancer more common in women with periodontal disease?
Indeed it is. There are meta-analyses on this topic that clearly show that breast cancer is associated with periodontitis.
Interestingly, a systematic review and meta-analysis suggest a significant link between oral Fusobacterium nucleatum species and their role in female breast cancer pathogenesis (Akbari et al, 2024). F. nucleatum could contribute to tumour development through several different mechanisms, such as production of cytokines and reactive oxygen species, which in turn can cause mutations and epigenetic changes. It was therefore hypothesized that targeting F. nucleatum could be beneficial in the therapy of breast cancer.
Can periodontitis also affect fertility in women?
Some studies have suggested that fertility is lower in women with periodontitis. However, further research and adequate statistical analyses are needed to confirm this correlation, as there is always the chance that common risk factors are largely responsible for it.
What mechanisms underlie the links between periodontal diseases and impaired health in women?
On the one hand, female sex hormones have a significant impact on periodontal tissues, thereby promoting periodontal diseases. On the other hand—as is understood for other associations between periodontal and systemic diseases—it is micro-organisms in the dysbiotic biofilm, their components and products, and inflammatory molecules from the inflamed periodontium that can affect women's health via the bloodstream. There is therefore a causal relationship. Common risk factors—such as smoking, age, socioeconomic status, heavy alcohol consumption, obesity, and other systemic diseases and conditions—also play a role in the association between periodontal diseases and impaired health.
Conclusion
Research shows that periodontitis is closely linked to women’s health. While common risk factors play a role in associations between periodontal disease and specific conditions, some true cause-and-effect relationships are also responsible.
Although periodontitis is associated with general diseases that occur in both men and women—such as cardiovascular disease, type-2 diabetes, and neurodegenerative diseases—there are also associations that occur only in women: gestational diabetes, premature birth, and breast cancer.
Women should be informed about these associations and motivated to maintain good oral hygiene and keep their check-up appointments. Periodontitis treatment is safe during the second trimester of pregnancy. And even with antiresorptive therapy for postmenopausal osteoporosis, periodontitis can be of successfully treated. Close co-operation between medical and dental professionals is essential for the well-being of our patients.
For further information, visit the EFP's Oral Health & Pregnancy campaign
Select bibliography
Akbari E, Epstein JB, Samim F. Unveiling the Hidden Links: Periodontal Disease, Fusobacterium Nucleatum, and Cancers. Curr Oncol Rep. 2024 Nov;26(11):1388-1397. doi: 10.1007/s11912-024-01591-w. Epub 2024 Aug 12. PMID: 39133417.
Gaba FI, González RC, Martínez RG. The Role of Oral Fusobacterium nucleatum in Female Breast Cancer: A Systematic Review and Meta-Analysis. Int J Dent. 2022 Nov 23;2022:1876275. doi: 10.1155/2022/1876275. PMID: 36466367; PMCID: PMC9711985.
Guo X, Yu K, Huang R. The ways Fusobacterium nucleatum translocate to breast tissue and contribute to breast cancer development. Mol Oral Microbiol. 2024 Feb;39(1):1-11. doi: 10.1111/omi.12446. PMID: 38171827.
Paz HES, Stolf CS, Bao K, Monteiro MF, Carvalho LM, Silbereisen A, Belibasakis GN, Casarin RCV, Bostanci N. The Subgingival Host-Microbial Landscape in Mothers With Periodontitis and Their At-Risk Offspring. J Clin Periodontol. 2025 Oct 2. doi: 10.1111/jcpe.70045. Epub ahead of print. PMID: 41038688.
Reis AA, Monteiro MF, Bonilha GM, Saraiva L, Araújo C, Santamaria MP, Casati MZ, Kumar P, Casarin RCV. Parents with periodontitis drive the early acquisition of dysbiotic microbiomes in their offspring. J Clin Periodontol. 2023 Jul;50(7):890-904. doi: 10.1111/jcpe.13815. Epub 2023 Apr 22. PMID: 37086047.
Salama M, Al-Taiar A, McKinney DC, Rahman E, Merchant AT. The impact of scaling and root planing combined with mouthwash during pregnancy on preterm birth and low birth weight: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2024 Nov 6;24(1):726. doi: 10.1186/s12884-024-06905-1. PMID: 39506741; PMCID: PMC11542403.
Shao J, Wu L, Leng WD, Fang C, Zhu YJ, Jin YH, Zeng XT. Periodontal Disease and Breast Cancer: A Meta-Analysis of 1,73,162 Participants. Front Oncol. 2018 Dec 12;8:601. doi: 10.3389/fonc.2018.00601. PMID: 30619743; PMCID: PMC6299876.
Shi T, Min M, Sun C, Zhang Y, Liang M, Sun Y. Periodontal disease and susceptibility to breast cancer: A meta-analysis of observational studies. J Clin Periodontol. 2018 Sep;45(9):1025-1033. doi: 10.1111/jcpe.12982. Epub 2018 Aug 9. PMID: 29974484.
Wang K, Zhang Z, Wang Z. Assessment of the association between periodontal disease and total cancer incidence and mortality: a meta-analysis. PeerJ. 2022 Nov 7;10:e14320. doi: 10.7717/peerj.14320. PMID: 36389427; PMCID: PMC9648345.
Wu J, Wu J, Tang B, Zhang Z, Wei F, Yu D, Li L, Zhao Y, Wang B, Wu W, Hong X. Effects of different periodontal interventions on the risk of adverse pregnancy outcomes in pregnant women: a systematic review and network meta-analysis of randomized controlled trials. Front Public Health. 2024 Sep 20;12:1373691. doi: 10.3389/fpubh.2024.1373691. PMID: 39371200; PMCID: PMC11449777.
Biographies
Professor James Deschner is director of the Department of Periodontology and Operative Dentistry at the University of Mainz, Germany, and is currently chair of the EFP’s scientific affairs committee. After graduating from the Free University of Berlin, he conducted research and worked at the Charité (Berlin), Cologne University, Bonn University, Pittsburgh University, and Ohio State University. In 2017, he was appointed the Noel Martin Visiting Chair in the Faculty of Dentistry at the University of Sydney, Australia.
Lisa Hezel is an experienced specialist in periodontology with a private practice in Magdeburg, Germany, and a research position at the University of Mainz in the Department of Periodontology and Operative Dentistry. She is actively involved in professional organizations, including the German Society of Periodontology—serving six years on the board—and the EFP as a member of the Communications Committee since 2022.




