
Issue No. 142
Summarized from Journal of Clinical Periodontology, Volume 52, Issue 10, October 2025, 1398-1409
Editor: James Deschner, chair, EFP scientific affairs committee
Beyond the probe: measuring patient satisfaction in periodontal therapy
Authors: Caspar Victor Bumm, Sophie Gaenesch, Florian Nagler, Iris Frasheri, Falk Schwendicke, Vinay Pitchika, Christina Ern, Richard Heym, Charlotte Wetzel, Matthias Folwaczny, Nils Werner
Background
Oral health-related quality of life (OHRQoL) has become an important outcome measure in dentistry, reflecting not only physical functioning but also psychological and social well-being. Periodontitis, a common chronic disease, profoundly affects these aspects of life. Symptoms such as tooth mobility, migration, bad breath, and eventual tooth loss may cause both functional impairment and aesthetic concerns, leading to reduced life satisfaction and social withdrawal.
Although patient-reported outcomes are increasingly emphasized, current periodontal therapy endpoints still rely heavily on clinical measures. For example, the EFP's clinical-practice guidelines propose strict thresholds to define treatment success in stages I–III periodontitis.
More recently, a more flexible treat-to-target (T2T) concept has been put forward, which allows limited residual pocketing—although still based solely on clinical measures.
These differing approaches highlight the challenge of aligning clinical definitions of periodontal stability with patient-centred outcomes such as OHRQoL.
Aim
To investigate if clinical outcomes and endpoints of periodontal treatment show any association with OHRQoL in long-term supportive periodontal therapy (SPT) patients.
Materials & methods
Study design:
Longitudinal follow-up study of patients treated in the undergraduate programme of the Department of Conservative Dentistry and Periodontology, University Hospital, Ludwig Maximilian University Munich, Munich, Germany.
Study population:
- Periodontitis patients treated between 2011–2016.
- Attending supportive periodontal therapy (SPT).
- Presented for re-examination in 2024.
Time points:
- T0: baseline: before step 1 and 2 of periodontal therapy.
- T1: periodontal re-evaluation, 6.33 ± 3.79 months after T0.
- T2: long-term re-examination, 126 ± 30 months (≈10 years) of SPT.
Study variables:
- T0, T1, T2: periodontal charting:
- Probing pocket depth (PPD).
- Bleeding on probing (BoP).
- Tooth mobility.
- Plaque.
- T2: additional examinations:
- OHRQoL measured with the German short version of Oral Health Impact Profile-14 (OHIP-14).
- Prosthetic status.
- Self-reported tooth migration.
- Compliance with SPT.
- Patient variables: age, gender, current smoking status, and diabetes mellitus.
Composite outcomes:
- EFP endpoint: no PPD >4mm with BOP, no deep pockets (≥6mm).
- T2T endpoint: ≤4 sites with PPD ≥5mm.
Statistical analysis:
- Linear regression to model the association between OHRQoL and endpoints adjusted for confounders (sex, smoking, diabetes, and SPT compliance).
- To increase the robustness of the assessment, the two investigated endpoints (EFP/T2T) were merged for regression analyses.
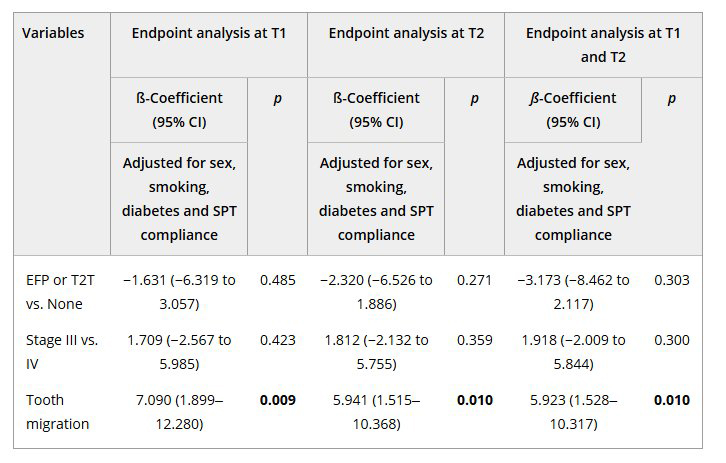
Note: Data are presented as β-coefficient with corresponding 95% confidence interval (CI). Bold indicates statistically significant values (p < 0.05).
Abbreviations: EFP, endpoint defined by Sanz et al. (2020); OHIP, oral health impact profile; SPT, supportive periodontal therapy; T1, 6.33 ± 3.79 months after step 2 therapy; T2, 126 ± 30 months after step 2 therapy; T2T, endpoint defined by Feres et al. (2020).
Results
Patient characteristics:
- Total patients: 47 (out of the 122 of the initial cohort of 759 who agreed to extended data processing).
- Mean age: 71.7 ± 10.5 years.
- Stages:
- Stage III: 40.4%.
- Stage IV: 59.6%.
- Smokers: 8.5%.
- Diabetes: 12.8%.
- SPT compliance:
- Regular attendance = 48.9%.
- Irregular attendance = 51.1%.
- Tooth migration: 25.5% reported.
- Tooth loss was minimal (median 1 over 10 years).
- Prosthetic status (28 Stage IV patients):
- Fixed: 46.4%.
- Removable: 39.3%.
- None: 14.3%.
Composite outcomes
- EFP endpoint achieved: 1 patient.
- T2T endpoint achieved: 16 patients.
- No endpoint achieved: 30 patients.
Patients failing endpointsshowed significantly more pockets and deep pockets at T2 (p < 0.001).
OHIP-14 scores – OHRQoL
- Mean total OHIP-14 score: 4.87 ± 6.38. This indicates a low OHRQoL impact.
- Eighty-three percent of the patients did not find life less satisfying because of their oral health, although12.8% reported occasional dissatisfaction.
- Stage IV patients reported higher overall OHIP-14 scores (5.79 ± 7.17) than those with Stage III (3.53 ± 4.86), especially concerning psychological discomfort and physical pain.
- Regarding the prosthetic status of Stage IV patients, the analysis revealed that those who had not received a prosthetic rehabilitation reported higher OHIP-14 scores (11.75 ± 9.14) than those with fixed (6.08 ± 7.97) or removable (3.27 ± 4.03) prostheses.
- Neither the achievement of clinical endpoints following steps 1 and 2 of therapy nor periodontal stability over the observation period was significantly associated with OHIP-14.
Regression analysis
Self-reported tooth migration was identified as a significant factor influencing OHIP-14 scores at T2 in all regression models.
Limitations
- OHRQoL was assessed only at the final follow-up (10 years), which prevents evaluation of temporal changes during therapy.
- The study had a small sample size (n = 47).
- Because of the patients’ characteristics, conclusions can be drawn only about stage III and IV periodontitis.
- The high mean age of the patients limits the generalisability of the findings.
- The monocentric, non-controlled design reduces external validity.
- Active periodontal therapy was performed by undergraduate students, potentially introducing operator-related variability despite specialist supervision.
- Only one patient achieved the EFP endpoint, limiting the statistical power for this criterion.
- Tooth migration was self-reported, without objective clinical verification, which may have introduced perception bias.
Conclusions and impact
- Achieving clinical endpoints of periodontal therapy (EFP and T2T) did not significantly improve patient-perceived OHRQoL.
- Despite clinical improvements, patients continue to report dissatisfaction and lower OHRQoL scores, particularly when tooth migration is present.
- This might suggest that clinical “success” does not always mean patient satisfaction.
- Residual aesthetic concerns highlight the need to address functional and aesthetic problems, especially in patients with advanced periodontitis.
- Patients with stage IV periodontitis and no rehabilitation tended to be more dissatisfied compared to stage IV periodontitis patients with prosthetic rehabilitation.
- Integrating patient-reported outcomes into periodontal research and translating this inro day-to-day care would allow therapy to be more tailored to the patients’ expectations and needs, improving quality-of-life outcomes.
When managing periodontitis, clinicians should therefore consider patients’ aesthetic and functional concerns, as well as their perceived oral-health wellbeing, as complementary measures of treatment success alongside clinical parameters.
Rapporteurs: Francesca Pacifico, Haitam Yousfi, and Zacharenia Zoi Zafeiriadou, supervised by Isabelle Laleman
Affiliation: Postgraduate programme in periodontoogy, University of Liège, Liège, Belgium
With kind permission from Wiley Online Library. Copyright © 1999-2025 John Wiley & Sons, Inc. All rights reserved




