
Issue No. 144
Summarized from Journal of Clinical Periodontology, Volume 52, Issue 12, December 2025, 1734-1745
Editor: James Deschner, chair, EFP scientific affairs committee
Collagen matrix maintains root coverage at three years
Authors: Lorenzo Tavelli, Shayan Barootchi, Maria V. Rodriguez, Leonardo Mancini, Hamoun Sabri, Tu Nguyen, Jad Majzoub, Suncica Travan, William V. Giannobile.
Background
Subepithelial connective tissue grafts (CTGs) are considered the standard approach for root-coverage procedures. However, the need for palatal harvesting is associated with increased surgical time and postoperative morbidity, particularly in cases involving multiple adjacent gingival recessions.
To overcome these limitations, xenogeneic collagen matrices (VCMX) have been proposed as alternative soft-tissue grafting materials. These matrices are volume-stable, readily available, and eliminate donor-site morbidity, while also serving as potential carrier scaffolds for biologically active molecules.
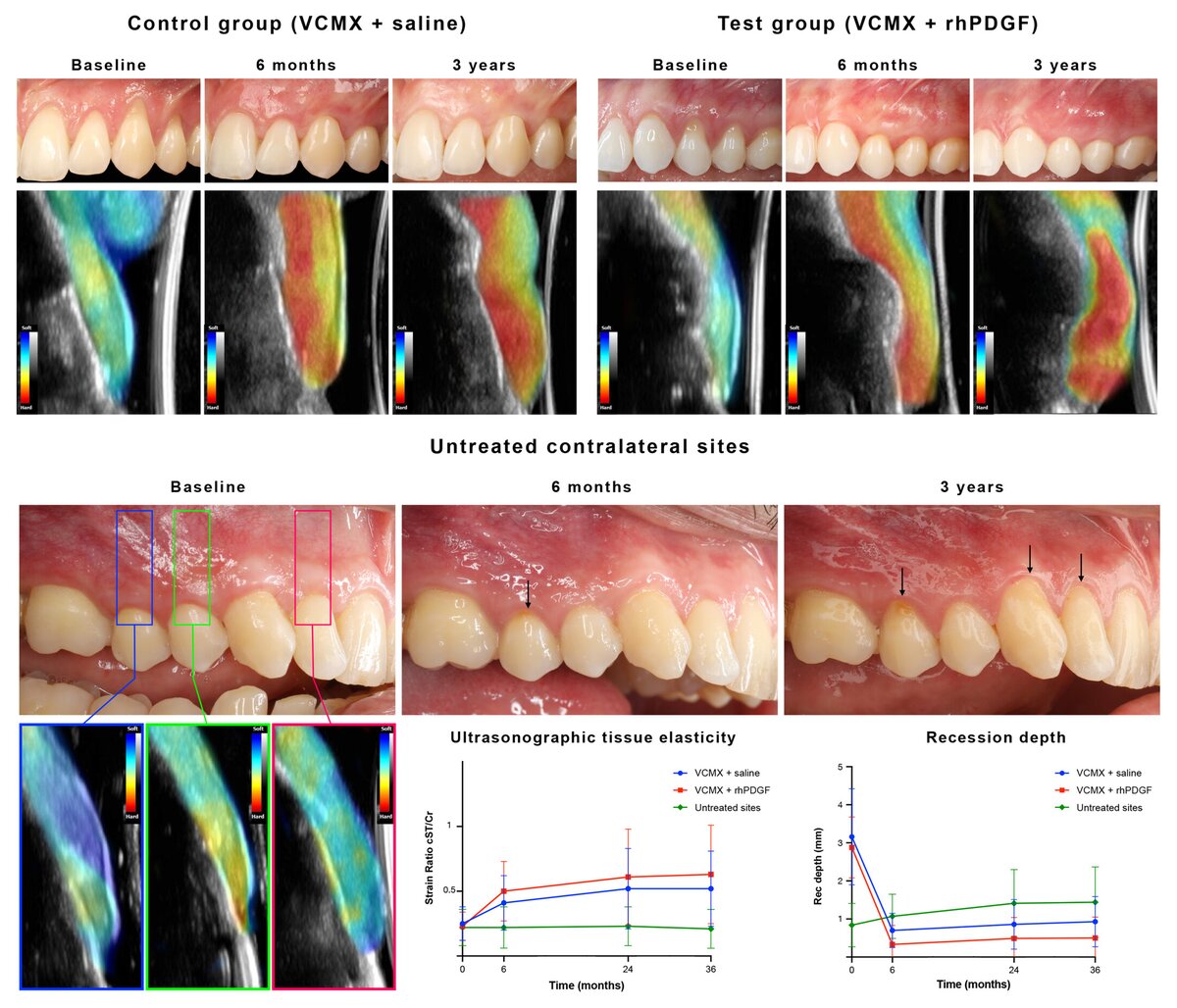
Recombinant human platelet-derived growth factor-BB (rhPDGF-BB) has been shown to promote angiogenesis and fibroblast activity and may enhance early wound healing when combined with collagen matrices. In a previously reported six-month randomized clinical trial, the adjunctive use of rhPDGF-BB was associated with improved early root coverage, aesthetic outcomes, and soft-tissue volume.1
Whether these initial advantages persist over time, and whether collagen matrix-based augmentation can provide stable long-term root coverage compared with untreated sites, has not yet been clearly established. The present three-year follow-up study was conducted to address these questions.
1. Tavelli, L., S. Barootchi, M. V. Rodriguez, et al. 2022. “Recombinant Human Platelet-Derived Growth Factor Improves Root Coverage of a Collagen Matrix for Multiple Adjacent Gingival Recessions: A Triple-Blinded, Randomized, Placebo-Controlled Trial.” Journal of Clinical Periodontology 49,11: 1169–1184. https:// doi. org/ 10. 1111/ jcpe. 13706.
Aim
This study evaluated three-year outcomes of gingival-recession treatment using a coronally advanced flap combined with a VCMX soaked in rhPDGF-BB or saline. The primary outcome was root-coverage stability from six months to three years. Secondary outcomes included clinical, aesthetic, patient-reported, and ultrasonographic parameters.
Materials & Methods
Study design
- Triple-blinded (patient, operator, and examiner), randomized, placebo-controlled clinical trial.
- Blinding procedures were maintained throughout the three-year follow-up period.
Participants
- Thirty patients with multiple adjacent gingival recessions were initially enrolled.
- 80 recession defects were included in the analysis.
- Each participant contributed at least two adjacent recession sites on the same side of the mouth.
Interventions
- All treated sites received a coronally advanced flap combined with a VCMX.
- In the test group, the VCMX was saturated with 1.5 mL of rhPDGF-BB.
- In the control group, the VCMX was soaked in sterile saline.
- The VCMX was trimmed extraorally, positioned over the exposed root surfaces, and stabilized beneath the coronally advanced flap.
- All participants received regular supportive periodontal care during the study period.
Outcome assessment and follow-up
- The primary outcome was mean root coverage at three years compared with the six-month evaluation.
- Secondary outcomes included complete root coverage, keratinized tissue width, probing depth, clinical attachment level, volumetric and aesthetic outcomes, patient-reported measures, and ultrasonographic assessment of tissue thickness, density, and elasticity.
- Clinical and ultrasonographic evaluations were performed at baseline, six months, one year, and three years.
- Untreated contralateral teeth were monitored as reference sites to assess natural recession progression.
Results
Participant flow
- Twenty-six of the 30 enrolled patients (87%) were available for evaluation at the three-year follow-up, resulting in 14 test subjects and 12 control subjects.
Root coverage outcomes
- Both treatment groups demonstrated a high degree of root coverage stability over the three-year observation period.
- Mean root coverage at six months was 78.6% in the control group and 88.5% in the test group, decreasing to 72.7% and 81.0%, respectively, at three years.
- The reduction in root coverage between six months and three years was limited and not statistically significant in either group.
- More than 90% of treated sites in both groups exhibited a stable gingival margin, defined as a change of ≤0.5mm over time.
- Longitudinal analyses across the full study period showed greater overall recession reduction, clinical attachment gain, mean root coverage, and complete root coverage in the rhPDGF-BB group; however, no significant intergroup differences were observed at the three-year time point.
Clinical, volumetric, and aesthetic outcomes
- Keratinized tissue width increased modestly but significantly in both groups.
- Probing depth and clinical attachment level remained stable over time.
- Aesthetic outcomes were favourable in both groups, with slightly higher final scores in the test group, although changes over time were comparable.
- Volumetric analyses showed minor, non-significant soft-tissue volume reductions between six months and three years, while overall volume and tissue thickness gains over the full follow-up period were greater in the test group.
Ultrasonographic and patient-reported outcomes
- Ultrasonographic assessment revealed increased tissue density and stiffness at treated sites in both groups, with no significant differences between treatments.
- Patient satisfaction and aesthetic perception remained high, and dentin hypersensitivity decreased significantly in both groups.
- In contrast, untreated contralateral sites showed progressive gingival recession and increased sensitivity over time.
Limitations
- Only 26 patients completed the three-year follow-up, so the study may be underpowered for detecting small differences between groups. Four patients (13%) were lost, which could bias results.
- All surgeries were performed by experienced specialists; results might differ in routine practice. A single type of implant system and surgical protocol was used, which may limit generalizability.
- The study did not include an autogenous graft group. While VCMX is a valid alternative, direct comparison to the CTG standard would clarify the relative efficacy over time.
- The economic impact of adding rhPDGF-BB was not assessed. Since PDGF is expensive, cost-benefit considerations for its routine use remain unknown.
- Only contralateral teeth were used as untreated references (not randomly assigned), which may introduce bias.
Conclusions and impact
- After three years, treated sites retained most of their coverage. Both groups showed minimal relapse in gingival-margin position, demonstrating that a cross-linked collagen matrix provides durable root coverage results in multiple recession defects.
- Although the rhPDGF-BB group had slightly higher overall coverage, there were no statistically significant differences between the groups at three years for mean or complete root coverage. In other words, adding PDGF did not yield a clear long-term advantage over saline-soaked matrix in this study.
- Both treatments led to thicker, denser tissue coronally (as measured by ultrasound), suggesting true tissue maturation. Patient-reported outcomes were similarly good.
- The untreated contralateral teeth became more recessed and sensitive, highlighting that, without intervention, gingival recessions tend to progress
Cross-linked collagen matrices, used with a coronally advanced flap, can achieve and maintain root coverage comparable to early postoperative results. Since both methods maintained coverage equally well by three years, clinicians may opt to use the matrix alone, potentially saving cost and the complexity of adding rhPDGF-BB. This biomaterial approach avoids donor-site surgery and provides a stable gingival outcome over the mid-term.
Rapporteurs: Lina Bakali, Sofie Caufriez, Alex Coman, Arthur De Ganck, Caroline Dequae, Britt Dupont, Pierre Lahoud, Maria Tsichlaki, Kato Van Caesbroeck, Jamin Van der Veken, Andy Temmerman, and Ana Castro. Supervised by Prof. Wim Teughels (programme director)
Affiliation: Postgraduate programme in periodontology, KU Leuven University, Leuven, Belgium
With kind permission from Wiley Online Library. Copyright © 1999-2025 John Wiley & Sons, Inc. All rights reserved




