
Issue No. 140
Summarized from Journal of Clinical Periodontology, Volume 52, Issue 8, August 2025, 1147–1157
Editor: James Deschner, chair, EFP scientific affairs committee
How effective is M-MIST plus collagen-enriched bovine xenograft for the treatment of intrabony defects?
Authors: Yuzhe Sun, Haidong Zhang, Churen Zhang, Xiaochi Chang, Hongqiao Zhao, Xiangyu Sun, Pierpaolo Cortellini, Kaining Liu, Jianxia Hou
Background
The modified minimally invasive surgical technique (M-MIST) used on its own has shown promising outcomes in treating intrabony periodontal defects.
However, studies evaluating the addition of adjunctive regenerative materials—such as deproteinized bovine bone minerals, enamel matrix derivatives (EMD), recombinant human platelet-derived growth factor, or platelet-rich fibrin—have reported similar clinical and radiographic advantages after both short-term and long-term follow-up.
However, these studies also showed limitations—such as limited effectiveness in space maintenance and clot stability—that may be related to certain inherent properties of the respective materials.
Hence, a collagen-enriched bovine-derived xenograft (CEBDX) may overcome some of these limitations and lead to better outcomes because of its superior mechanical properties.
Although some studies have utilized CEBDX in periodontal regeneration, there are no published data from controlled clinical studies testing the hypothesis that utilizing CEBDX materials could enhance the outcomes of M-MIST in the treatment of intrabony periodontal defects.
Aim
This randomized clinical study aimed to investigate if the addition of CEBDX offers superior clinical and radiographic outcomes compared to M-MIST alone in treating intrabony periodontal defects.
Materials & methods
Study Population
- About three months after the completion of steps 1 and 2 of periodontal therapy, 40 non-smoking patients with stage III or IV periodontitis and an isolated residual intrabony defect were included in the study.
- Full-mouth plaque score and full-mouth bleeding score had to be less than 30%.
- Isolated intrabony defects were at least 3mm, with a probing depth ≥ 5mm.
- The residual intrabony defects were two-wall, three-wall, or two-to-three-wall morphologies.
- No furcation defects were included.
Intervention
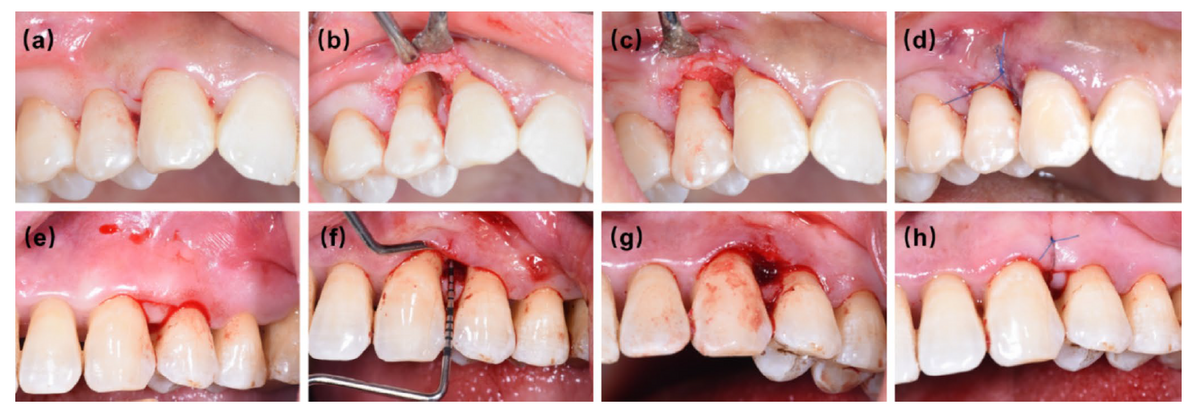
- The patients were randomly assigned to two groups: test group (M-MIST combined with CEBDX) and control group (M-MIST alone).
- All surgical procedures were performed by an experienced masked periodontal surgeon. Two independent masked dentists performed the clinical examinations and statistical analyses.
- During the surgery, the anatomy of the defect, probing depth (PD), clinical attachment level (CAL)—from buccal/labial side (CAL-B) and from lingual/palatal side (CAL-L)— were examined and recorded by the operator, as well as the distance from the top of the gingival papilla to the interproximal contact point (DTPCTP).
- PD, CAL, DTPCTP, and radiographic bone volume were measured at one- and two-year follow-ups.
- The radiographic bone-volume changes of the defects were evaluated by periapical radiographs and cone beam computed tomography (CBCT).
- Univariate analyses were carried out to test the correlation between the independent variables (including all measured clinical parameters) and the primary outcome variable, CAL-B gain at the two-year follow-up.
Results
Clinical outcomes
- One patient in each group (two in total) was lost to follow-up.
- No post-operative complications were reported in either of the groups.
- The test group achieved approximately 1mm greater pocket reduction compared to the control group after two years at the buccal aspect of the defect (3.95 ± 1.39 mm in the test group vs 2.95 ± 1.51 mm in the control group, p = 0.041).
- The test group gained approximately 1mm greater CAL compared to the control group at the buccal side of the defect (3.58 ± 1.31 mm vs. 2.53 ± 1.81 mm, p = 0.043).
- There was no statistically significant difference in DTPCP.
- There was no statistically significant difference in terms of PD or CAL at the lingual aspects.
- There were no sites with residual PD ≥ 6mm in either of the groups after the two-year observation.
Radiographic outcomes
- The mean radiographic vertical bone level (RBL) gain in the test group was higher than the RBL gain in the control group (1.68 ± 1.86 mm vs. 0.93 ± 1.34 mm, respectively) at the two-year follow-up, but this difference did not reach a statistical significance.
- Bone volume gain was higher in the test group compared to the control group (17.77 ± 11.44 mm3 vs 8.63 ± 7.10 mm3, p = 0.011).
- The result of multiple linear-regression analyses indicated that the baseline buccal clinical attachment level significantly affected the amount of buccal CAL gain observed after two years.
- The addition of CEBDX resulted in a 1.013mm (95% CI: 0.110–1.917 mm) gain in the buccal CAL at the two-year follow-up after adjusting for confounding factors.
Limitations
- Both groups included a very limited number of molar teeth (only one in the test group and two in the control group). The results may therefore not be applicable to multi-rooted teeth.
- The control group had shallower mean PDs at baseline compared to the test group (5.26 mm vs 6.16 mm) on the buccal aspects, which may have contributed to the greater pocket reduction after the surgery in the test group.
- The validity of the CBCT analysis for assessing bone-volume gain remains uncertain.
- Additional higher bone gain for the test group could be attributed to the presence of residual xenograft not being absorbed or replaced, as the provided data do not distinguish between the xenograft particles and new bone formation.
- Other limitations include the lack of histological confirmation of regeneration, the small sample size, and the lack of longer-term follow-up.
Conclusions and impact
- M-MIST, with or without CEBDX, is an effective treatment modality to improve clinical and radiological outcomes of regenerative periodontal therapy in isolated residual intrabony defects.
- M-MIST with CEBDX resulted in an additional 1mm gain in CAL in two-wall, three-wall, and two-to-three-wall intrabony defects after two years.
This study may assist practitioners in selecting an appropriate biomaterial to use in conjunction with the M-MIST technique for periodontal regeneration. However, given the modest improvements in clinical and radiographic outcomes, the cost-benefit of utilizing these biomaterials should be carefully considered.
Rapporteur: Roya Safi, supervised by Assoc. Prof. Ryan Lee (co-director) and Prof. Savo Ivanovski (director)
Affiliation: Postgraduate programme in periodontology,University of Queensland, Australia
With kind permission from Wiley Online Library. Copyright © 1999-2025 John Wiley & Sons, Inc. All rights reserved




