
Issue No. 145
Summarized from Journal of Clinical Periodontology, Volume 53, Issue 1, January 2026, 2-11
Editor: James Deschner, chair, EFP scientific affairs committee
Tooth loss in treated advanced periodontitis after more than 20 years of supportive care
Authors: Thomas Eger, Felix Wörner, Neelam Lingwal, Peter Eickholz
Background
Tooth loss is considered a true end point of many clinical studies in dentistry. Patients with periodontitis are more susceptible to tooth loss, particularly those diagnosed with stages III and IV of the disease. The aim of periodontitis treatment is to maximize the longevity of teeth, although it is accepted that not every tooth can be saved from extraction.
Morbidity from periodontitis-associated tooth loss is an increasing issue for patients, with these individuals often requiring complex prosthodontic rehabilitation. The restoration of function for patients diagnosed with stage III/IV periodontitis may include the use of removable, fixed partial, or implant-supported fixed partial dentures.
The most appropriate long-term treatment modality for partially edentulous patients with periodontitis remains unclear. As the global population ages, identifying optimal prosthodontic rehabilitation strategies is becoming increasingly necessary.
Aims
This retrospective study aimed to evaluate long-term tooth loss in a cohort of German military personnel patients with treated generalised stage III/IV periodontitis after at least 20 years of supportive periodontal care. It compared those with no or minimal prosthodontic treatment (control) to those with fixed partial dentures, implant-supported fixed partial dentures, and tooth-supported removable dentures. The study also sought to determine the 10-year survival rate of these different types of dentures.
Materials and methods
- Study design
- Retrospective cohort study (1993-2013).
- Prospective observational extension (2014-2023) for continued monitoring with no new interventions.
- Total observation period:1993-2023 (30 years).
- Study setting
- Single-centre study at Department XXIII Dentistry-Periodontology, Bundeswehr Central Hospital (German Armed Forces Central Hospital), Koblenz, Germany.
- This department served as a specialist periodontal treatment centre for military personnel.
- Population
- Military personnel with stage III/ IV periodontitis who underwent specialist periodontal treatment.
- Patients not adhering to supportive periodontal care (SPC) protocol were excluded.
- Medical screening included diabetes status, smoking, and systemic conditions affecting periodontal outcomes.
- Methods/Data collection
- Periodontal therapy
- Oral-hygiene instruction and motivation.
- Full-mouth non-surgical periodontal therapy.
- Periodontal reassessment and surgical treatment (where indicated).
- Selective use of systemic antibiotics according to contemporary guidelines.
- All patients were enrolled in individually tailored SPC programmes following active therapy.
- Prosthetic allocation based on first major rehabilitation received:
- Tooth-supported fixed partial dentures (≥5 units and supported by teeth only) (FPDs).
- Removable metal partial dentures retained with clasps (RPDCs).
- Removable metal partial dentures retained with double crowns (RPDDs).
- Implant-supported fixed partial dentures (iFPDs).
- Control group had no major prosthesis (FPD with <5 units, no RPD, ≤2 implants) after active periodontal therapy.
- Baseline defined as completion of active periodontal therapy (for control group) or insertion of first prosthesis (prosthetic groups).
- Periodontal therapy
- Outcome measures
- Primary outcome: tooth loss during SPC period (excluding third molars).
- Secondary outcome: 10-year survival of prosthetic restorations.
- Statistical analysis
- Tooth loss analysed using negative binomial regression models.
- Prosthetic survival after 10 years analysed using logistic regression.
- Patient-level analysis adjusted for confounders (e.g. age, smoking).
Results
- Population
- 233 patients with stage III/IV periodontitis.
- 21% females (n=49).
- 74.2% (n=173) stage III and 25.8% (n=60) stage IV periodontitis.
- Mean follow-up: 21.7±2.7 years (range: 10-29 years) after active periodontal therapy.
- 70% (n=163) of patients were completely adherent to SPC.
- Tooth loss (TL):
- Patients with major restorations (n=101) had significantly higher annual TL rates (0.24±0.33 teeth/year) than controls (n=132).
- Stage IV patients experienced higher average TL compared with stage III patients: 0.22±0.27 versus 0.11±0.23 teeth/ year respectively (p=0.001).
- TL rates by prosthesis type:
- RPDCs: 0.4±0.39 teeth/year (mean follow-up 23.2±3.1 years).
- RPDDs: 0.35±0.42 teeth/year (mean follow-up 24.2±2.6 years).
- FPDs: 0.23±0.33 teeth/year (mean follow-up 23.8±3 years).
- iFPDs: 0.15±0.22 teeth/year (mean follow-up 23.8±2.9 years).
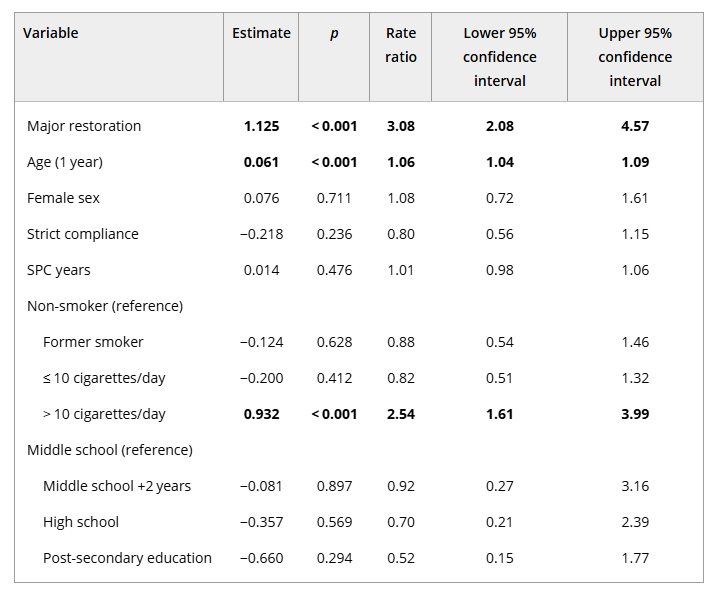
- Risk factors which significantly contributed to rate of TL in general:
- Age (RR 1.06, 95% CI 1.04-1.09, p<0.001).
- Smoking >10 cigarettes a day (RR 2.54, 95% CI 1.61-3.99, p<0.001).
- Major restoration (RR 3.08, 95% CI 2.08-4.57, p<0.001).
- 10-year survival rates of different types of dental restorations:
- FPDs demonstrated the highest prosthetic survival rate at 93% in 90% of patients.
- 83% of iFPD in 76% of patients.
- 75% of RPDDs in 80% of patients.
- 67% of RPDCs in 75% of patients.
Limitations
- Internal validity:
- Selection bias in observational study design.
- The imbalance in group sizes and baseline characteristics restricted direct comparability between treatment groups.
- Tooth loss could not always be attributed exclusively to periodontal causes (losses because of caries or trauma may have occurred).
- Adherence to SPC may have varied over time despite inclusion criteria, potentially influencing long-term results.
- Baseline characteristics of study groups (controls versus major restorations) were unevenly distributed for key aspects such as smoking, periodontitis stage, and mean number of teeth at baseline. This may have biased results.
- External validity:
- Generalizability is limited, as findings may not be transferable beyond a military population with mandatory dental care.
- Within the German context, military personnel underwent mandatory dental examinations and received more intensive dental care than the general population, which may limit extrapolation to civilian settings.
- Female participants were underrepresented, further constraining broader applicability.
Conclusions and impact
- After active treatment, patients diagnosed with stage III/IV periodontitis enrolled in an SPC programme who received prosthetic rehabilitation displayed a higher long-term tooth-loss rate compared with control-group patients who received no or minimal prosthetic intervention.
- No statistically significant differences were identified between the control group and the implant group with regards to average tooth loss rate during SPC.
- Mean tooth loss was statistically significantly associated with age and heavy smoking (>10 cigarettes/day).
This study provides long-term evidence on tooth loss in patients treated for advanced periodontitis undergoing prosthetic rehabilitation. Analysis over up to three decades highlights the potential influence of prosthetic design on tooth retention in a high-risk population and underscores the importance of risk-factor control and lifelong supportive periodontal care.
Rapporteurs: Shen Deng Fam, June Teh, and Beant Thandi, supervised by Prof. Jacopo Buti and Assoc. Prof. Natalie Leow
Affiliation: Postgraduate programme in periodontology, UCL Eastman Dental Institute, London, UK
With kind permission from Wiley Online Library. Copyright © 1999-2026 John Wiley & Sons, Inc. All rights reserved




