
Issue No. 141
Summarized from Journal of Clinical Periodontology, Volume 52, Issue 9, September 2025, 1298-1305
Editor: James Deschner, chair, EFP scientific affairs committee
What factors help long-term survival of teeth with Class II furcation involvement?
Authors: P. Eickholz, T. Cordis, B. Dannewitz, B. Pretzl, M. Schröder, N. Lingwal, N. El Sayed
Background
Maintaining natural teeth in function has been, and remains, the main goal of dentistry and periodontology. Evidence has shown that multirooted teeth represent a greater challenge because of anatomical tooth-related factors that can sometimes make it difficult to obtain a complete and proper plaque control.
Clinical evidence has shown that a class II furcation involvement (FI) in mandibular molars and buccal maxillary molars can be treated by regenerative surgery, obtaining closure or even a grade I FI after surgery. But this is not the case for an interproximal class II FI, as no specific treatment (surgical or non-surgical) has yet been proven to give a clinical advantage.
Moreover, there is still a lack of information—regarding all the factors that could influence the long-term retention of class II FI molars—to guide the clinician in the treatment decision and provide some clinical data about the likely future survival of the tooth.
Aim
This retrospective cohort study aimed to collect and analyse the factors that could explain the long-term prognosis of molars with class II FI.
Materials and methods:
- Patients with at least one tooth with Class II FI who underwent active periodontal therapy (APT) since October 2004 at the Centre for Dentistry and Oral Medicine of Goethe University Frankfurt, Germany.
- Patients underwent subgingival instrumentation and supportive periodontal care performed by undergraduate dental students, supervised by postgraduate dentists specializing in periodontology. All surgical interventions were performed by the postgraduate dentists.
- Each patient’s perio chart and radiographs were carefully analysed at baseline (T0), after completion of APT (first or second re-evaluation) and start of supportive periodontal care (T1), and five years or more after the completion of APT (T2).
- The main outcome of the study was tooth loss during supportive periodontal care.
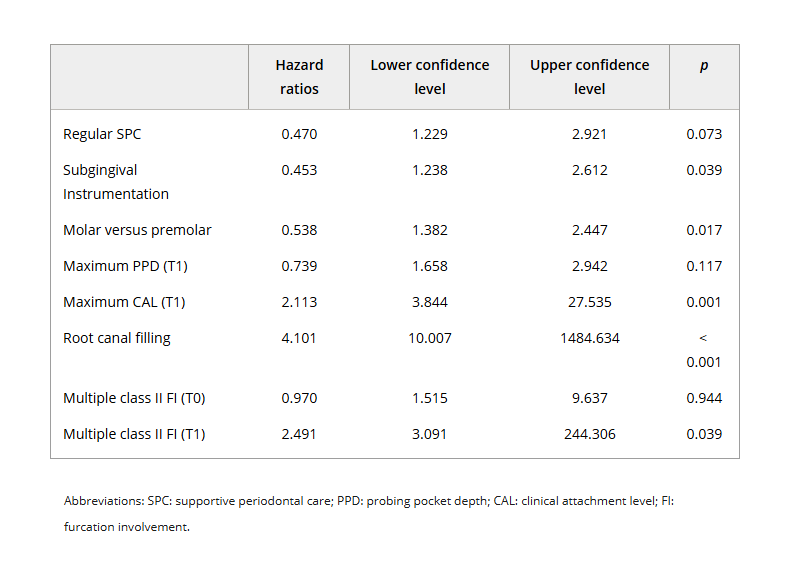
- Statistical analysis: univariate chi-square tests were performed, and a logistic mixed-model regression together with a mixed Cox proportional hazard model were applied.
Results
- A total of 222 patients participated, presenting 543 multirooted teeth with class II FI.
- Patient level: During APT, 16 teeth were extracted, while 93 were extracted during SPC over 10 years. Teeth were extracted because of caries, endodontic or periodontal problems, or prosthetic reasons (for 10 teeth, the indication for extraction could not be assessed). Seventeen patients had diabetes, 35 were active smokers, and 32 received adjunctive systemic antibiotics. Patient characteristics were not related at any point to tooth loss.
- Tooth level:
- Twenty-eight of the 543 teeth were first maxillary premolars and 515 teeth were molars.
- More teeth were lost if they had multiple rather than single class II FI at T0 and T1, root-canal filling, or higher CAL and PPD at T1.
- From T0 to T1: 181 teeth went from FI class II to FI class I, 19 progressed to class III FI, and 327 remained stable.
- From T1 to T2: 105 teeth improved, 85 deteriorated, and 243 remained stable.
- Treatment:
- One hundred and forty-four teeth received step 3 treatment, while 400 were treated only by steps 1 and 2.
- Univariate comparisons showed that teeth treated by subgingival instrumentation showed less tooth loss.
- Roots resected in resective treatment did not show statistical significance.
- The models showed less tooth loss for molars compared with premolars, and where regular SPC was performed. On the other hand, CAL, multiple class II FI per tooth at T1, and root-canal fillings were associated with greater tooth loss.
Limitations
- A retrospective design inherently carries a high risk of bias because of its reliance on past data.
- Because the final group was small, not all surgical treatments could be analysed because of underpowering.
- The single-centre data collection could also be considered a limitation because the number of teeth treated by surgical and non-surgical approaches at this centre might not reflect the reality of other centres.
- A clear and adequate comparison between surgical and non-surgical treatment cannot be made because of the difference in the number of teeth that underwent each specific treatment.
- Even if, in the present study, patient-related factors did not show an association, it does not mean they should be overlooked.
Conclusions and impact
- Periodontal treatment can lead to long-term tooth survival.
- The presence of multiple FI class II at the start of SPC is a strong indicator for tooth loss.
- Supportive periodontal care is important—results showed it to be a positive factor for less tooth loss—but it is not enough in itself. Factors including root-canal fillings, multiple furcation involvement, premolars, and CAL all have a negative impact on the long-term retention of teeth.
- Nonetheless, the above conclusion should be treated with a degree of caution, as there was a significant difference in the number of teeth treated in step 2 and step 3 of the therapy.
This study supports and underlines the importance of the treatment of teeth with FI class II and the value of SPC for long-term retention, emphasizing tooth retention and long-term survival.
Rapporteur: Melanie Llerena, supervised by Prof. Mario Aimetti (programme director)
Affiliation: Postgraduate programme in periodontology, University of Turin, Italy
With kind permission from Wiley Online Library. Copyright © 1999-2025 John Wiley & Sons, Inc. All rights reserved




