
Issue No. 138
Summarized from Journal of Clinical Periodontology, Volume 52, Issue 6, June 2025, 826–835
Editor: James Deschner, chair, EFP scientific affairs committee
What is the longevity and effectiveness of cross-arch bridges in patients with stage III/IV periodontitis?
Authors: Øystein Fardal and Jostein Grytten
Background
Managing patients with stage III or IV periodontitis often involves long-term maintenance following the initial active periodontal therapy. Despite proper treatment, some patients experience progressive tooth mobility and loss.
For these patients, cross-arch bridges may offer both tooth replacement and stabilization of the dentition. Not without controversy, implants have been used as added support to stabilize bridges.
While previous studies have shown the feasibility of such bridges, data on their long-term outcomes—including failure rates, prognostic indicators, and patient satisfaction—are limited.
Furthermore, questions remain regarding how well these bridges prevent further tooth loss and whether combining implants with teeth used as abutments poses risks.
The EFP’s clinical-practice guideline on the treatment of stage IV periodontitis recommends such bridges under specific conditions.
Aim
To evaluate the long-term outcomes of cross-arch stabilizing bridges in patients with stage III and stage IV periodontitis, including failure rates, risk factors of failure, their effectiveness in preserving abutment teeth, and patients’ satisfaction levels, over up to 35 years of clinical follow-up.
Material and methods
- Study design: Retrospective clinical study conducted in a private Norwegian periodontal practice.
- Population: 94 patients (57 females, 37 males) with 111 cross-arch bridges placed between 1986 and 2016 (representing 1.7% of the total patient population on a maintenance programme).
- Inclusion criteria:
- Diagnosed with stage III/IV periodontitis.
- Received active periodontal therapy (steps 1–3, according to the EFP guidelines).
- Cross-arch fixed bridgework spanning at least from canine to canine.
- Bridges constructed on teeth or on a combination of teeth and implants.
- Minimum follow-up of seven years.
- Bridge types:
- 90 tooth-supported bridges.
- 21 tooth-implant combination bridges.
- Bridge span: Mean 10.2 units (range: 6–14).
- Follow-up:
- Mean patient follow-up: 24.2 years
- Mean bridge observation: 17.9 years
- Dropouts and deceased patients were accounted for, with reasons for dropouts recorded.
- Assessments:
- Periodontal probing and radiographs every five to six years.
- Technical/biological complications were recorded (caries, continued periodontal breakdown, traumatic events, fractures, gingival retractions/aesthetic problems, endodontic complications).
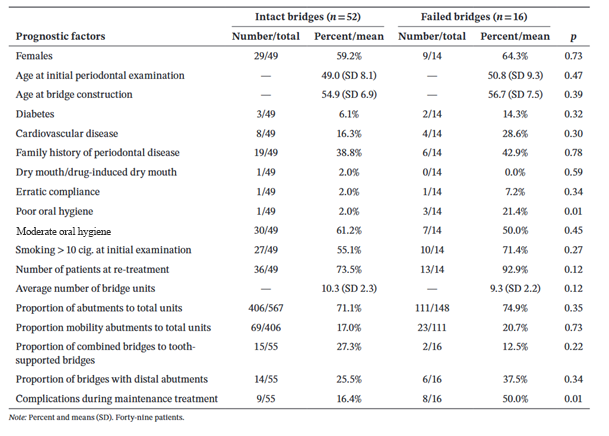
- Prognostic factors for losing bridges were analysed, including oral-hygiene status, smoking habits, and compliance with maintenance programmes.
- Patient-satisfaction interviews about the bridges in terms of function, aesthetics, and/or discomfort.
- Data analysis: Descriptive statistics, chi-2 test, t-test, Mann-Whitney U test; significance at p<0.05.
Results
- Bridge failure rate: 14.4% (16 out of 111 bridges) after an average of 16.1 years. Most common failure causes: caries, periodontal breakdown, trauma.
- Tooth loss from the bridges was significantly lower (8.9%) for the abutment teeth compared to the same arch not covered by dental bridges (34.4%) and the teeth in the opposing arch (25.4%).
- Abutment teeth had significantly better retention (p<0.0001).
- Bridge design findings:
- 37 bridges had distal cantilevers; six (16%) failed after 14.2 years.
- 21 were tooth–implant supported; 3 (14%) failed, with two implants lost and six cases of peri-implantitis.
- Risk factors: Significant predictors of failure were poor oral hygiene (p=0.0093) and maintenance complications (p=0.0059).
- Patient satisfaction: Generally high, with minimal concerns, even in the presence of aesthetic compromises.
Limitations
- The retrospective design of the study limits control over data collection and potential confounders.
- The comparison between tooth loss in the bridges and the remaining teeth in the same arch may be misleading, as the bridges typically spanned more than 10 units, primarily leaving molars unbridged, and these are teeth that are inherently more prone to loss.
- Only a small proportion of patients had poor oral hygiene, possibly weakening the statistical conclusion.
- The practice is exclusive to periodontology, with very closely monitored patients, which may limit the external generalizability.
- The sample size is limited because only a few highly selected patients have been rehabilitated with this type of bridge.
Conclusions and impact
- Cross-arch bridges constructed for patients with stage III/IV periodontitis show long-term success and tooth preservation, with a failure rate of only 14.4% after an average of 16 years.
- Poor oral hygiene and complications during maintenance therapy were significant prognostic factors for bridge failure.
- Combining teeth and implants did not have a negative effect on the success of these bridges, as the failure rate was 14.0%.
- Distal cantilevers showed a slightly higher failure but remained clinically acceptable.
- The bridges effectively reduced further tooth loss, with significantly lower tooth loss from the bridges compared to the same and opposing arches.
- Patient satisfaction was high, with most patients content with the function and aesthetics of the bridges.
For selected patients with advanced periodontitis, cross-arch stabilizing bridges are a viable long-term solution to prevent further tooth loss and maintain oral function, as long as they maintain good oral hygiene and have regular maintenance therapy. The integration of these bridges into treatment planning could offer an alternative to implant-only approaches.
Rapporteur: Alexandros Svestonof supervised by Marjolaine Gosset and Laurent Detzen.
Affiliation: Postgraduate programme in periodontology, Paris Cité University, France.
With kind permission from Wiley Online Library. Copyright © 1999-2025 John Wiley & Sons, Inc. All rights reserved




