Publications Hub, Public health & Prevention, Systemic health, Article
The association between periodontitis and erectile dysfunction—how can periodontists help improve men’s health?
19 November 2025
There is solid evidence of an association between periodontitis and erectile dysfunction and some evidence that the relationship is causal. Furthermore, studies have shown that periodontal treatment can have a positive effect on reducing the severity of erectile dysfunction, although more research is needed. James Deschner (chair, EFP scientific affairs committee) and Lisa Hezel (member, EFP communication and engagement committee) weigh up the evidence and highlight other aspects of gum health related to men.
What is the evidence for the association between periodontitis and erectile dysfunction?
Several meta-analyses published in the last 10 years have shown that there is indeed a link between periodontitis and erectile dysfunction (Farook et al., 2021; Zhou et al., 2019; Liu et al., 2017; Wang et al., 2016). On average, these analyses found that male patients with periodontitis were two to three times more likely to experience erectile dysfunction.
However, care should be taken when interpreting the results of these meta-analyses: the included studies were very heterogeneous and erectile dysfunction was almost always assessed using self-administered questionnaires (e.g., the International Index of Erectile Function or the Sexual Health Inventory for Men), rather than objective methods such as Doppler ultrasound. Nevertheless, it can be concluded that there is an association between periodontitis and erectile dysfunction.
Given that erectile dysfunction is associated with obesity, diabetes mellitus, and cardiovascular disease—which are all also associated with periodontitis—and the presence of common risk factors, such as age and smoking, how is it possible to be clear that periodontitis alone is associated with erectile dysfunction?
That is a very good, but also very complex, question. Of course, there are many other diseases and conditions associated with erectile dysfunction. For instance, high blood pressure, cardiovascular disease, dyslipidaemia, poorly controlled diabetes, and obesity have been linked to erectile dysfunction. Smoking, chronic heavy alcohol consumption, low socioeconomic status, and older age are also linked to erectile dysfunction.
As these conditions also increase the risk of periodontitis, part of the association between periodontitis and erectile dysfunction could result from these shared risk factors. Studies therefore attempt to exclude, control for, or statistically adjust for such common risk factors where possible in order to better understand the relationship between periodontitis and erectile dysfunction. However, there may also be unknown or not yet fully understood risk factors influencing this relationship.

Photo: Shutterstock
Are we talking merely about association or is there evidence of a causal relationship?
Recognizing an association between two diseases can also be helpful, even if it is only based on common risk factors and no causality exists. This could enable preventive measures against the second disease to be taken as soon as the first disease occurs. Of course, a causal link between the two diseases—periodontitis and erectile dysfunction in this case—would be even more significant, as we could then directly influence the risk of erectile dysfunction by preventing, diagnosing, and treating periodontitis.
Many of the currently known links between periodontal and systemic diseases are not only related to shared risk factors but also to a causal relationship. This means that periodontitis itself contributes to systemic diseases, and vice versa. There is therefore a bidirectional relationship. However, proving a causal relationship is difficult. Even longitudinal studies are not sufficient evidence, as the occurrence of one disease before the other does not prove that it is responsible for the subsequent disease. A helpful way to establish causality is to conduct an intervention study in which one disease is treated and then examined to see whether this also leads to changes in the second disease.
Regarding the link between periodontitis and erectile dysfunction, there is some evidence—though so far not very much—that periodontitis could directly contribute to erectile dysfunction. This means that there could indeed be a causal relationship. Interestingly, there is also debate as to whether causality could run in both directions. For instance, erectile dysfunction could negatively impact self-confidence, stress levels, and social activities, which could in turn lead to poorer or neglected oral hygiene and thus an increased risk of periodontal diseases.
Is there any evidence that periodontal treatment alone can have a positive effect on erectile dysfunction?
Yes, at least two intervention studies have been performed, in which periodontitis was treated and erectile dysfunction was recorded at the beginning and end of the study (El-Makaky et al., 2020; Eltas et al., 2013). In the study by El-Makaky et al., 140 patients with periodontitis and erectile dysfunction were randomly assigned to either the control group or the test group, both of which had 70 participants. Erectile dysfunction was assessed at the beginning of the study and again after three months of therapy. The study by Eltas et al. involved 120 patients with erectile dysfunction and periodontitis. The treatment and control groups each comprised 60 patients. Erectile dysfunction was assessed at the beginning of the study and one and three months after treatment.
Both studies showed that periodontal therapy led to an improvement in erectile dysfunction, as measured by a questionnaire. As previously mentioned, it would have been preferable to assess erectile dysfunction using Doppler ultrasound. It is also unclear whether the positive effect of periodontal therapy on erectile dysfunction is long-lasting. Nevertheless, it is encouraging that such intervention studies have been conducted. Further research is needed to confirm these results and provide a definitive conclusion regarding causality.
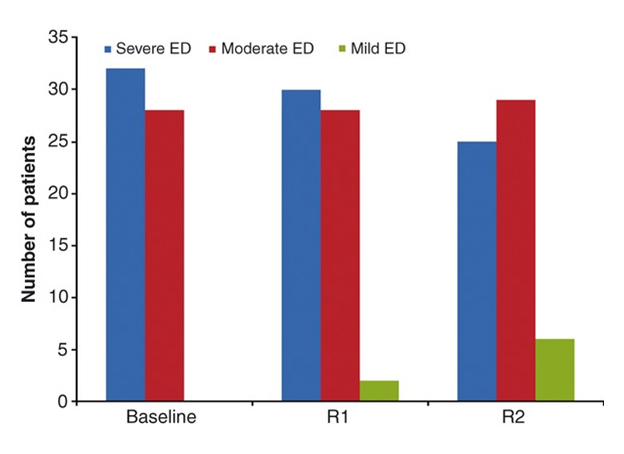
(IIEF, International Index of Erectile Dysfunction; ED, Erectile dysfunction; R1, one month after; R2, three months after.)
From: Eltas A, Oguz F, Uslu MO, Akdemir E. The effect of periodontal treatment in improving erectile dysfunction: a randomized controlled trial. J Clin Periodontol. 2013 Feb;40(2). © John Wiley & Sons, Inc.
What are the theories and evidence, on the mechanisms by which periodontitis may contribute to erectile dysfunction?
In periodontitis, microorganisms, their components and products, and inflammatory molecules enter the systemic circulation. They can thus cause direct and indirect damage, including vascular damage, in other parts of the human body. Periodontitis is known to be associated with a worsening of early markers of atherosclerosis, such as endothelial function, intima-media thickness, and pulse-wave velocity. Conversely, treatment of periodontitis can lead to an improvement in these markers.
Therefore, it is reasonable to hypothesise that periodontitis could also impair penile vessel function. Erectile dysfunction is characterized by reduced dilatation of the penile vessels. Nitric oxide is necessary for dilatation, and therefore for blood flow, in the penile vessels; however, the nitric-oxide concentration decreases in the presence of oxidative stress. Atherosclerotic changes, which are promoted by proinflammatory cytokines, also lead to a decrease in dilatation and blood flow in the penile vessels. Through inflammatory molecules and oxidative stress, periodontitis could therefore contribute to vascular erectile dysfunction.
Beyond erectile dysfunction, what is the evidence linking periodontitis (or poor oral health in general) to reduced sperm quality, infertility, etc.?
Several studies have examined the link between periodontitis and sperm quantity and quality, finding that sperm concentration may be lower in men with periodontitis. There is also some evidence that periodontitis may alter sperm morphology and reduce motility. Common risk factors also certainly play a role in these associations. It would be particularly exciting if intervention studies could demonstrate that treating periodontitis improves sperm count and quality. This could potentially motivate some male patients to practise adequate oral hygiene and, if necessary, seek treatment for periodontitis.
In terms of treatment, what are the implications of the latest research? What needs to be done in terms of greater collaboration between periodontists/dentists and general practitioners and sexual-health specialists?
To promote interdisciplinary cooperation in this area, greater interest and commitment needs to be generated among general practitioners and specialists in sexual health. Joint professional events, consensus papers, podcasts, and videos could be valuable tools for raising awareness and encouraging discussion. Medical and dental professionals should educate their male patients about the links between oral health and men's health. Medical-history forms could include specific questions on this topic to help identify potential risks early on. Mutual referrals for affected patients should be facilitated. Finally, interdisciplinary research between urology, fertility clinics, and dentistry departments at universities must be expanded to gain new scientific insights for the benefit of patients.
An important consideration is that the topic of erectile dysfunction is still often taboo, or at least considered somewhat embarrassing, so it tends to be avoided or approached with humour, which does not do justice to the seriousness and suffering of those affected. Because of the link to periodontitis, this topic needs to be addressed openly and professionally in dental practices, as happens in the case of oral health in connection with pregnancy and women's health.
What other areas are relevant in terms of the relationship between periodontal health and men’s health?
Another interesting topic related to oral health and men's health is testosterone. Testosterone levels in men naturally decline with age. It is debated whether this decline could be linked to an increased risk of periodontitis in older age. Testosterone primarily has anti-inflammatory effects, but the inhibitory effect of testosterone on inflammation may be lost with age, resulting in an overly strong and prolonged immunological inflammatory response to a periodontal microbial attack. However, further studies are needed for a definitive assessment. Additionally, several meta-analyses have revealed an association between periodontitis and prostate cancer (Guo et al., 2021; Wie et al., 2021; Ma et al., 2020; Corbella et al., 2018).
Finally, it should also be noted that certain risk factors for periodontitis are more pronounced in men. For example, men tend to have lower health awareness, less adequate oral hygiene, and are more likely to have unhealthy diets and smoking habits. Overall, the studies show that there are significant links between oral health and general health in men. It is therefore important that we discuss these links, conduct more extensive and in-depth research, and educate our patients.
Select bibliography
Corbella S, Veronesi P, Galimberti V, Weinstein R, Del Fabbro M, Francetti L. Is periodontitis a risk indicator for cancer? A meta-analysis. PLoS One. 2018 Apr 17;13(4): e0195683. doi: 10.1371/journal.pone.0195683. PMID: 29664916; PMCID: PMC5903629.
El-Makaky Y, Abdalla Hawwam S, Hifnawy T. Salivary tumor necrosis factor-alpha to detect the severity of erectile dysfunction: A randomized clinical trial. Oral Dis. 2020 Oct;26(7):1548-1557. doi: 10.1111/odi.13380. Epub 2020 Jul 20. PMID: 32367561.
Eltas A, Oguz F, Uslu MO, Akdemir E. The effect of periodontal treatment in improving erectile dysfunction: a randomized controlled trial. J Clin Periodontol. 2013 Feb;40(2):148-54. doi: 10.1111/jcpe.12039. Epub 2012 Dec 17. PMID: 23252455.
Farook F, Al Meshrafi A, Mohamed Nizam N, Al Shammari A. The Association Between Periodontitis and Erectile Dysfunction: A Systematic Review and Meta-Analysis. Am J Mens Health. 2021 May-Jun;15(3):15579883211007277. doi: 10.1177/15579883211007277. PMID: 34013796; PMCID: PMC8142012.
Guo Z, Gu C, Li S, Gan S, Li Y, Xiang S, Gong L, Wang S. Periodontal disease and the risk of prostate cancer: a meta-analysis of cohort studies. Int Braz J Urol. 2021 Nov-Dec;47(6):1120-1130. doi: 10.1590/S1677-5538.IBJU.2020.0333. PMID: 33650836; PMCID: PMC8486441.
Liu LH, Li EM, Zhong SL, Li YQ, Yang ZY, Kang R, Zhao SK, Li FT, Wan SP, Zhao ZG. Chronic periodontitis and the risk of erectile dysfunction: a systematic review and meta-analysis. Int J Impot Res. 2017 Jan;29(1):43-48. doi: 10.1038/ijir.2016.43. Epub 2016 Nov 10. PMID: 27829669.
Ma H, Zheng J, Li X. Potential risk of certain cancers among patients with Periodontitis: a supplementary meta-analysis of a large-scale population. Int J Med Sci. 2020 Sep 12;17(16):2531-2543. doi: 10.7150/ijms.46812. PMID: 33029095; PMCID: PMC7532473.
Wang Q, Kang J, Cai X, Wu Y, Zhao L. The association between chronic periodontitis and vasculogenic erectile dysfunction: a systematic review and meta-analysis. J Clin Periodontol. 2016 Mar;43(3):206-15. doi: 10.1111/jcpe.12512. Epub 2016 Mar 3. PMID: 26749274.
Wei Y, Zhong Y, Wang Y, Huang R. Association between periodontal disease and prostate cancer: a systematic review and meta-analysis. Med Oral Patol Oral Cir Bucal. 2021 Jul 1;26(4):e459-e465. doi: 10.4317/medoral.24308. PMID: 33247563; PMCID: PMC8254894.
Zhou X, Cao F, Lin Z, Wu D. Updated Evidence of Association Between Periodontal Disease and Incident Erectile Dysfunction. J Sex Med. 2019 Jan;16(1):61-69. doi: 10.1016/j.jsxm.2018.11.007. PMID: 30621927.
Biographies
Professor James Deschner is director of the Department of Periodontology and Operative Dentistry at the University of Mainz, Germany, and is currently chair of the EFP’s scientific affairs committee. After graduating from the Free University of Berlin, he conducted research and worked at the Charité (Berlin), Cologne University, Bonn University, Pittsburgh University, and Ohio State University. In 2017, he was appointed the Noel Martin Visiting Chair in the Faculty of Dentistry at the University of Sydney, Australia.
Lisa Hezel is an experienced specialist in periodontology with a private practice in Magdeburg, Germany, and a research position at the University of Mainz in the Department of Periodontology and Operative Dentistry. She is actively involved in professional organizations, including the German Society of Periodontology—serving six years on the board—and the EFP, where she is a member of the communications and engagement committee.




