Treatment, Article
What options are available to clinicians for crown-lengthening surgery
03 February 2026
In a preview of his presentation at Perio Master Clinic 2026 in Baku on March 6, Juan Blanco explains crown-lengthening surgery and the various options that are available to periodontists.
The clinical crown is defined as the portion of the tooth that is exposed to the oral environment, extending beyond the gingival or mucosal margin. A reduction in clinical crown height may occur because of occlusal or incisal wear, extensive carious destruction, traumatic fractures, or an altered position of the gingival margin located coronally to the cementoenamel junction.
In such situations, restorative treatment becomes particularly challenging. An insufficient clinical crown may compromise the establishment of adequate resistance and retention form for restorations, limit access to subgingival carious lesions, and hinder the achievement of satisfactory aesthetic outcomes. Furthermore, restorations placed too close to the alveolar crest may violate the supracrestal tissue attachment, leading to inflammation, attachment loss, or bone resorption.
Clinical crown lengthening is a well-established therapeutic procedure aimed at increasing the amount of exposed tooth structure to facilitate restorative procedures or to address aesthetic concerns. From a clinical perspective, crown lengthening procedures can be classified as either functional or aesthetic, depending on the primary treatment objective.
Functional crown lengthening is primarily indicated to expose subgingival caries, fractures, or restorative margins, thereby allowing proper isolation, margin placement, and long-term periodontal health. In contrast, aesthetic crown lengthening is mainly performed to correct excessive gingival display during smiling or to manage gingival enlargement that interferes with oral hygiene.
This aesthetic indication is most frequently encountered in the anterior sextants and is commonly associated with conditions such as delayed passive eruption. Aesthetic crown lengthening aims to improve the appearance of short clinical crowns while preserving the integrity of the supracrestal tissue attachment, traditionally referred to as the biologic width.
Achieving a harmonious relationship between teeth, gingiva, and lips—often described as the balance between “white” and “pink” aesthetics—is particularly critical in the anterior maxilla. In this region, functional and aesthetic objectives frequently converge, as restorative demands must be reconciled with high aesthetic expectations. An inappropriate gingival margin position or disproportionate tooth dimensions can significantly affect smile aesthetics and patient satisfaction.
Several surgical and orthodontic techniques are available to achieve clinical crown lengthening, including gingivectomy, apically positioned flaps with or without osseous resection, and orthodontic extrusion (forced eruption) either as a standalone procedure or in combination with surgical approaches. The selection of the most appropriate technique depends on multiple factors, including the position of the alveolar bone crest, the amount of keratinized tissue, the tooth’s restorative prognosis, and the aesthetic zone involved.

Gingivectomy (see Figure 1) is a surgical procedure that involves the excision of supracrestal gingival tissue while maintaining the integrity of the supracrestal tissue attachment. This technique is indicated when the distance between the planned gingival margin and the alveolar bone crest is at least 3mm, making flap elevation unnecessary. Gingivectomy is commonly performed using a scalpel, electrosurgery, or laser devices, each tool offering specific advantages in terms of precision, haemostasis, and postoperative comfort. However, gingivectomy is limited to cases in which osseous recontouring is not required and where sufficient keratinized tissue remains after surgery.
Apically positioned flap surgery with osseous resection (see Figure 2) is generally indicated when the alveolar bone crest is located closer than 3mm to the desired gingival margin. This approach allows direct visualization of the underlying bone architecture and facilitates precise bone removal. Osseous resection may include osteoplasty (which reshapes non-supporting bone) and ostectomy (which involves the removal of supporting bone directly associated with the tooth via the periodontal ligament). The primary objective of this procedure is to reposition the supracrestal tissue attachment more apically, thereby increasing clinical crown height while maintaining periodontal stability.

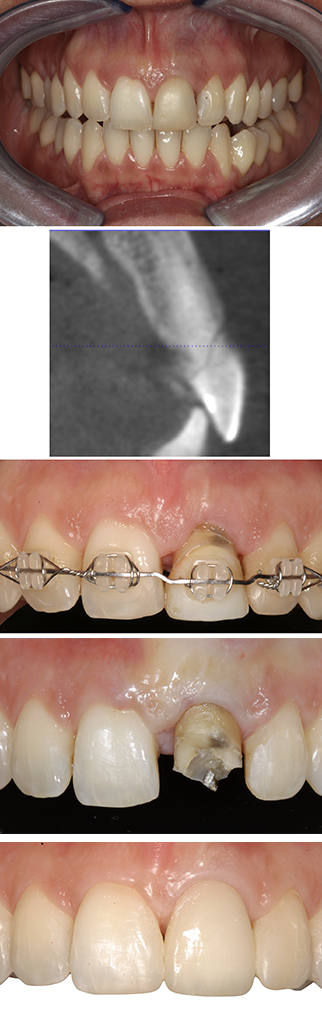
Orthodontic extrusion (see Figure 3), which is also known as forced eruption, represents an alternative or adjunctive approach in the management of teeth with deep subgingival defects. This technique is particularly valuable when surgical crown lengthening would require excessive removal of supporting bone, potentially compromising the periodontal support of adjacent teeth. Forced eruption is especially indicated in cases of root fractures, internal or external root resorption, isolated periodontal defects, or non-restorable teeth in aesthetically sensitive areas. By gradually extruding the tooth coronally, sound tooth structure can be exposed while preserving the alveolar bone and gingival architecture of neighbouring teeth.
Biography

Juan Blanco is professor and chair of the Department of Periodontology in the School of Medicine and Dentistry at the University of Santiago de Compostela in Spain, where he is also director of the master’s degree in periodontology and implantology and director of the continuing education programme in periodontology. He was president of the EFP in 2016-17, president of the Spanish Society of Periodontology (SEPA) from 2007 to 2010, and president of the Iberian section of the International Team for Implantology (ITI) from 2010 to 2016. He has also served as a member of the ITI’s international research commit (2015-2013) and as a member of the board of the Oral Reconstruction Foundation (2022-2024).
Perio Master Clinic is a triennial EFP conference designed specifically for dental clinicians. Taking place in Baku, Azerbaijan, Perio Master Clinic 2026 on the “Perio-Restorative Interplay” will offer participants the latest evidence-based clinical techniques in periodontology, implantology, and restorative dentistry. The scientific programme, featuring 29 speakers and moderators from 12 countries, emphasizes a multidisciplinary approach and will explore innovative products and techniques that provide predictable, aesthetic, and durable results for even the most complex cases.




