Treatment, Article
Why good wound healing is crucial to the success of periodontal and implant surgery
04 December 2025
In a preview of his presentation at Perio Master Clinic 2026 in Baku, Otto Zuhr explains the importance of good wound healing to the success of periodontal and implant surgery.
The successful execution of periodontal and implant surgical procedures essentially requires good wound healing. In reconstructive periodontal and implant surgery, rapid postoperative healing without complications is particularly important, not least because these interventions frequently involve the use of soft- and hard-tissue grafts or other replacement materials.
Bacterial contamination of these augmentation materials during the early stages of wound healing must be prevented in any case if the goal of undisturbed incorporation into the surrounding tissue is to be safely achieved.
In view of the oral microflora, prevention of bacterial contamination is only possible if primary wound closure occurs, so that healing takes place in a closed environment that is difficult for microorganisms to enter. This is often complicated by the fact that one of the two wound margins is constituted of the rigid, avascular surface of the tooth root or implant surface, neither of which typically offers favourable conditions for smooth wound-healing processes.
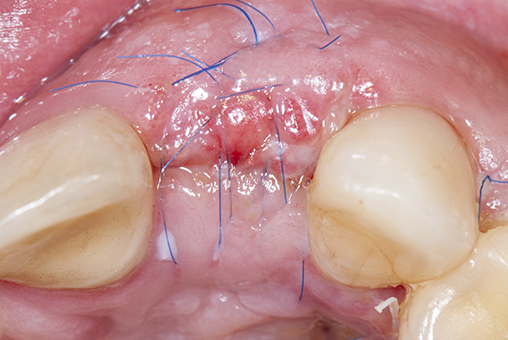
Therefore, achieving primary wound healing after surgery is considered the greatest challenge of periodontal and implant procedures as well as a decisive measure of success, in most cases aiming to avoid wound dehiscence, tissue defects, fibrotic-tissue formation, and scarring (Figure 1).
Wound healing encompasses all physiologic processes involved in restoring the integrity of injured body tissues. Since in nearly all surgical procedures the wounds are created by the surgeon—as opposed to trauma-induced wounds—there is a significant degree of control over many factors that are crucial for successful healing, both during wound creation and subsequent wound closure.
Patient- and defect-related wound-healing factors can only be indirectly influenced by appropriate patient selection and defect selection, it is primarily the technique-related factors that give the clinician the ability to directly influence the wound-healing process and, thus, the success of treatment.
According to the scientific literature, these factors include various surgical factors—such as incision technique, surgical flap type and thickness, tension-free surgical flaps, the volume of augmentation materials, the amount of tissue trauma caused by the procedure—as well as the manual dexterity of the surgeon.
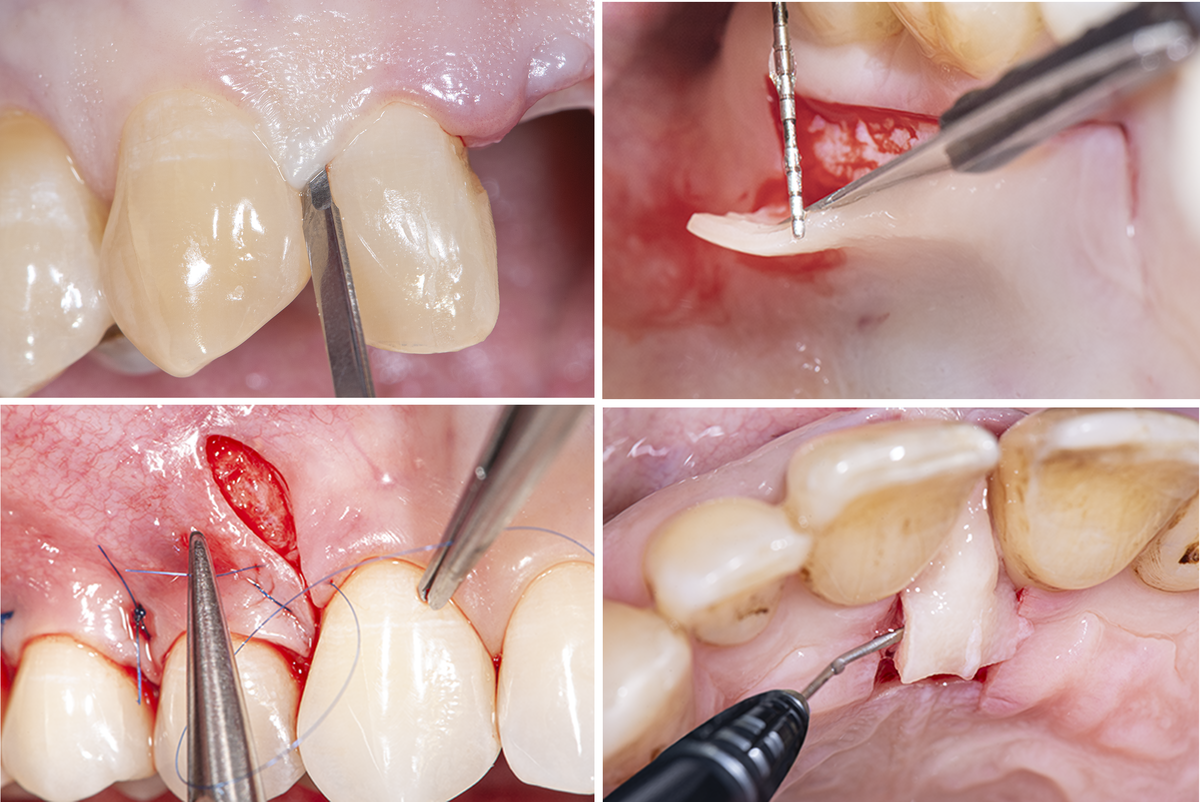
The quality of surgical soft-tissue management plays a decisive role in this context. Careful preoperative planning of all aspects of the procedure from the initial incision to flap preparation, flap mobilization, and flap stabilization is imperative. Measures to maintain the best-possible blood supply to the surgical area and to achieve the highest-possible wound stability are the focus of these efforts (Figure 2).
In this respect, a microsurgical approach with the use of optical magnification, microsurgical instruments, and microsurgical suture materials has scientifically proven advantages, and is today even considered indispensable from a clinical point of view.
The benefits of a precise and atraumatic treatment approach—which include significantly reduced morbidity, better clinical outcomes, and higher patient satisfaction regarding the procedure, as well as aesthetic treatment results such as scar-free healing, natural appearance, and harmonious tissue transitions—are becoming increasingly evident (Figure 3).

- Otto Zuhr will give the presentation “Structural biology of the dento-gingival complex. Principles of surgical wound healing” in the opening session of Perio Master Clinic 2026 on Friday 6 March, Surgical and Restorative Treatments for Smile Enhancement.
Perio Master Clinic is a triennial EFP conference designed specifically for dental clinicians. Taking place in Baku, Azerbaijan, Perio Master Clinic 2026 on the “Perio-Restorative Interplay” will offer participants the latest evidence-based clinical techniques in periodontology, implantology, and restorative dentistry. The scientific programme, featuring 29 speakers and moderators from 12 countries, emphasizes a multidisciplinary approach and will explore innovative products and techniques that provide predictable, aesthetic, and durable results for even the most complex cases.
Biography

Otto Zuhr studied dentistry at the University of Aachen from 1986 to 1992. He is board-certified specialist in periodontology of the German Society of Periodontology (DGParo) and runs a private office dedicated to periodontology and implant dentistry together with Marc Hürzeler in Munich, Germany. With more than 25 years of clinical experience and teaching practice, Dr Zuhr has become a proven expert in his field well beyond the European borders. He is an associate professorship position at the department of periodontology of the Johann-Wolfgang-Goethe University in Frankfurt/Main, Germany, and was a board member of DGPar from 2007 to 2014. Otto Zuhr has written several refereed scientific articles in the field of periodontology and implant dentistry and his book Plastic Esthetic Periodontal and Implant Surgery was published by Quintessence in 2012. His research activities are focused on oral soft-tissue wound healing and reconstruction.




