Publications Hub, Public health & Prevention, Systemic health, Article
Periodontitis: The overlooked cardiovascular risk factor
28 September 2025
World Heart Day (29 September) reminds us that prevention remains the most powerful tool in reducing the global burden of cardiovascular diseases (CVD). While much attention is rightly focused on diet, smoking, and hypertension, one common potential risk factor continues to be overlooked, despite a growing and robust body of scientific evidence: periodontitis. Francesco D’Aiuto highlights the latest research.
Periodontitis is a chronic inflammatory disease of the gums that affects over 40% of adults globally and, in its severe form, is one of the leading causes of tooth loss. But its impact extends far beyond the oral cavity. Periodontitis is now recognised as a chronic non-communicable disease with consequences that reach into vascular biology, metabolic control, immune function, and—crucially—cardiovascular health.
The growing evidence base: From association to causation
Over the past two decades, research—including from our group at the UCL Eastman Dental Institute—has revealed consistent epidemiological associations between periodontitis and CVD, including myocardial infarction, stroke, and peripheral artery disease. Meta-analyses have confirmed that people with periodontitis are at increased risk of future cardiovascular events, independent of traditional risk factors.
Biologically, this link is underpinned by shared inflammatory pathways. Patients with periodontitis consistently exhibit elevated systemic markers—such as C-reactive protein (CRP), interleukin-6, and tumour necrosis factor-alpha—as well as endothelial dysfunction, a well-established early marker of vascular injury and predictor of future atherosclerosis.
Periodontal pathogens such as Porphyromonas gingivalis have been identified in atherosclerotic plaques, and experimental models show that oral infection can trigger vascular inflammation and oxidative stress.
But a key question remained: can treating gum disease actually modify vascular risk?
A key strength of the EFP’s approach in recent years has been to integrate not only observational data but interventional evidence into clinical practice guidelines. In particular, the EFP-commissioned systematic review on the effects of periodontal treatment on systemic health1—which our group led—formed a critical evidence pillar in the development of consensus recommendations regarding the systemic impact of therapy (e.g., biomarkers, vascular function, inflammatory mediators). On that basis, the EFP has embedded these insights into its clinical guidelines, ensuring that evidence of systemic benefit is not an afterthought but an element of the rationale for periodontal therapy. The 2022 EFP guideline for stage IV periodontitis acknowledges that, beyond its role in restoring function, periodontal therapy may have beneficial systemic effects.
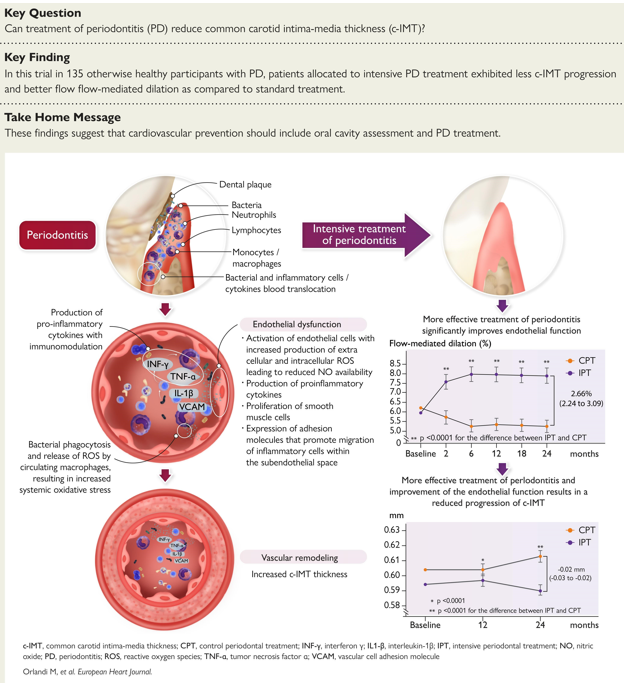
(From Orlandi et al, 2025; © the authors; published by Oxford University Press on behalf of the European Society of Cardiology).
Our group’s recent randomized controlled trial published in the European Heart Journal2 contributes importantly in this context—not as a standalone proof, but as a piece of emerging interventional evidence consistent with what the EFP review anticipated. In otherwise healthy individuals with severe periodontitis, intensive periodontal therapy was associated with:
- Reduction in carotid intima-media thickness (cIMT),
- Improved endothelial function (flow-mediated dilation),
- Declines in inflammatory and oxidative stress markers,
- Changes occurring independent of blood pressure, cholesterol, or weight shifts.
These findings align with, rather than contradict, the patterns predicted by meta-analyses and the EFP’s evidence synthesis.
Why does this matter for cardiovascular prevention?
The implications are far-reaching. Atherosclerosis begins silently and early, often decades before the first heart attack or stroke. During this subclinical phase, inflammation plays a key role in initiating and accelerating vascular damage. By treating periodontitis—a chronic, bacteria-driven source of systemic inflammation—we may be able to mitigate this process upstream. This positions periodontal care not only as a matter of oral health but also as a legitimate form of cardiovascular risk reduction. It reinforces the concept of the “oral-systemic connection” and demands greater collaboration between dental and other medical professionals.
Integrating oral health into cardiovascular risk assessment
Despite these findings, oral-health assessments remain absent from most cardiovascular guidelines and rarely feature in routine medical consultations. Conversely, dental professionals often lack the training, systems, or referral networks to flag patients with cardiovascular risk factors.
There is now a clear rationale for integrating basic periodontal screening into cardiovascular prevention pathways, particularly for patients with diabetes, metabolic syndrome, or a family history of CVD. Likewise, dental teams should be encouraged—and empowered—to identify patients at risk and refer them for medical follow-up. This bidirectional flow of information and care is central to the future of integrated, preventive healthcare. By situating periodontal care within cardiovascular prevention—not as peripheral but as complementary—we can shift paradigms: from seeing dentistry as downstream care to incorporating oral health into upstream risk management.
A call to action for World Heart Day
On this World Heart Day, let us broaden our vision: healthy gums are not a luxury—they are a key to healthy blood vessels.
- Policymakers should consider including oral health in national cardiovascular prevention policies.
- Clinicians and researchers should push for integration rather than siloed care.
- Patients and the public should be empowered to understand that bleeding gums are more than a nuisance—they may signal deeper systemic risk.
By referencing the EFP’s own clinical guidelines, the science now supports a bold yet pragmatic vision: treating periodontitis may not only protect teeth but also safeguard vascular health. As researchers, clinicians, and advocates, we must seize this moment—aligning oral health strategy with cardiovascular prevention to make “heart health” truly holistic.
References
1. Marco Orlandi, Eva Muñoz Aguilera, Debora Marletta, Aviva Petrie, Jean Suvan, Francesco D'Aiuto Impact of the treatment of periodontitis on systemic health and quality of life: a systematic review. J Clin Periodontol. 2022 Jun;49(Suppl 24):314‑327, doi:10.1111/jcpe.13554
2. Marco Orlandi, Stefano Masi, Ersilia Lucenteforte, Devina Bhowruth, Marco A Malanima, Ulpee Darbar, Kalpesh Patel, Chong Lim, Chiara Curra, Tay Shiehfung, Jeanie Suvan, Scott T Chiesa, John Deanfield, Francesco D’Aiuto, Periodontitis treatment and progression of carotid intima-media thickness: a randomized trial, European Heart Journal, 2025; ehaf555, https://doi.org/10.1093/eurheartj/ehaf555
Biography

Francesco D’Aiuto is Professor of Periodontology and Honorary Consultant at UCL Eastman Dental Institute and University College London Hospitals. He leads a multidisciplinary research programme investigating the connections between periodontal and systemic diseases, particularly cardiovascular and metabolic conditions. He has authored over 160 peer-reviewed publications, coordinates international clinical trials, and has contributed to several EFP S3-level clinical guidelines. He currently serves as President of the IADR Periodontal Research Group and holds advisory roles across European consortia and translational health ventures.




