Issue No. 129
Summarised from Journal of Clinical Periodontology, Volume 51, Issue 9, September 2024, 1122-1133
Editor: Andreas Stavropoulos, chair, EFP scientific affairs committee
Decision-making on using systemic antibiotics to treat periodontis
Authors: Patrizia C. Winkler, Leander Benz, Katrin Nickles, Hari C. Petsos, Peter Eickholz, Bettina Dannewitz
Background
The management of periodontitis, a chronic inflammatory condition affecting the supporting structures of teeth, often involves the use of systemic antibiotics as an adjunct to mechanical subgingival instrumentation. The decision to administer antibiotics is traditionally based on the presence of specific bacteria such as Aggregatibacter actinomycetemcomitans (A.a.) or guided by the severity of the disease and patient age. However, the indiscriminate use of antibiotics is discouraged because of growing concerns about antibiotic resistance. This study aims to evaluate the clinical outcomes of two decisionmaking strategies: one based on microbiological testing (i.e., the presence of A.a.) and the other on clinical factors (i.e., patient age and pocket probing depth, PPD).
Aim
To retrospectively compare the clinical effectiveness and the frequency of antibiotic usage between two different decision-making strategies in the management of periodontitis.
Materials & methods
- Study design: Retrospective analysis of medical records of patients treated between 2008 and 2018.
- Patient cohort: 425 patients treated for periodontitis at Goethe University in, Frankfurt, Germany.
- Interventions:
- Subgingival mechanical instrumentation of periodontal pockets.
- Adjunctive delivery of systemic amoxicillin and metronidazole based on detection of A. actinomycetemcomitans (A.a.+).
- Reclassification of cases based on the new staging and grading classification for periodontitis (2018) and administration criteria based on severity of periodontitis and/or patient age (i.e., <56 years and PPD ≥5mm in ≥35% of sites, or <36 years). - Outcome measures: Reduction in percentage of teeth with PPD ≥6mm at re-evaluation.
- Statistical analysis: Chi2 test for agreement on data between groups, Kruskal-Wallis test for intergroup differences.
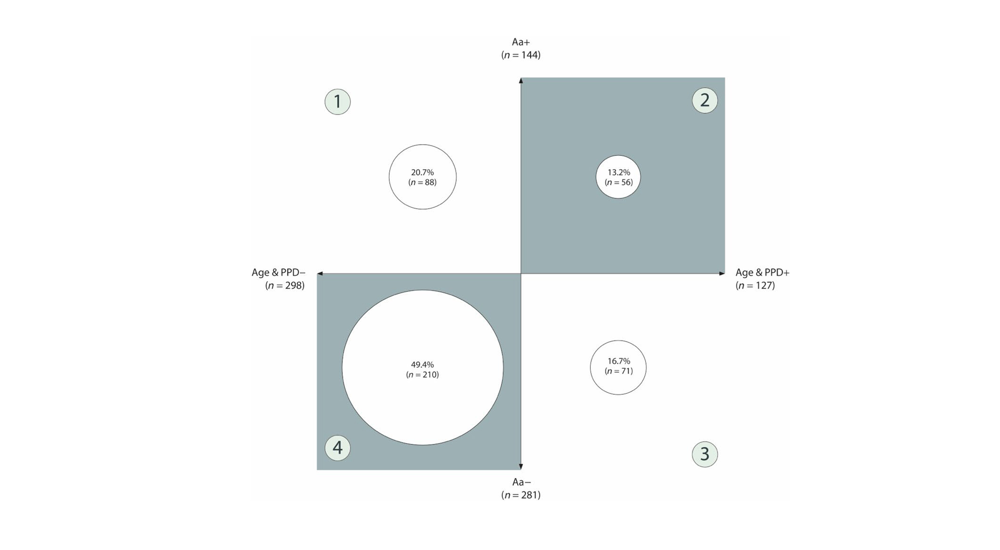
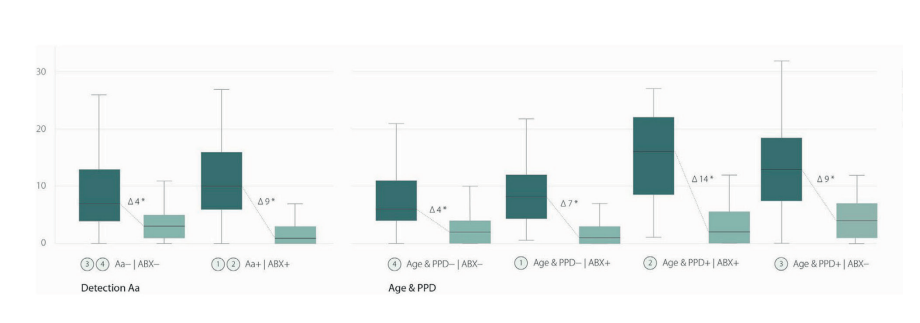
Note: Only 33.9% tested positive for Aggregatibacter actinomycetemcomitans (Aa+) and received antibiotics as adjunct to subgingival instrumentation. The cohort was retrospectively categorized according to the new approach based on age and disease severity (Age & PPD). Only 56 cases of Aa+ patients would also have been given antibiotics following the Age & PPD concept (group 2, 38.9% of Aa+). The agreement was slightly higher for cases that should not receive antibiotics under either concept (group 4, 74.7% of Aa−). However, the overall agreement between the two approaches was low (phi coefficient 0.14; p = .004). Eighty‐eight patients (group 1) who were treated with antibiotics based on their microbiological test result (Aa+) would not have received this treatment under the new concept (Age & PPD−), while 71 patients (group 3) who were Aa negative (Aa−) would have been recommended antibiotics based on their age and the severity of their disease (Age & PPD+).
therapy (T0) and at the time of re-evaluation after non-surgical treatment (T1).
Note: The study cohort was categorised according to whether antibiotics (ABX) were administered and whether the criteria for detection of Aa and age and severity of disease (Age & PPD) were met.
Results
- Patient profiles: 33.9% were A.a.+ and 29.9% met the age and PPD criteria.
- Clinical outcomes: Both approaches limited antibiotic use effectively, with the age and PPD group showing a greater reduction in deep periodontal pockets compared to the A.a.+ group.
- Agreement between approaches: Low agreement between the two methods, with significant differences in patient profiles selected for each approach.
- Characteristics of groups:
– 98.4% of patients in age & PPD group were classified as grade III-IV stage C periodontitis, while 81.3% were classified as such in the Aa+ group. The percentage of sites with PPD ≥5mm was 41.2% in the age and PPD group compared to 27% in the A.a.+ group. Thus, patients of the age & PPD group showed a greater extent and severity of disease compared to the A.a.+ group.
– Patients of the first group were also younger on average, were more likely to be smokers (34% vs. 22%), and showed fewer signs of metabolic disease such as diabetes mellitus (4% vs. 9%), compared to the A.a.+ group. - Outcomes differences between groups: Patients in the age & PPD group who also received antibiotics showed the greatest clinical improvement of all groups (14 fewer teeth less with PPD ≥6mm). The age & PPD group without antibiotics showed comparable results to the A.a.+ with antibiotics group (an average of nine fewer teeth with PPD ≥6mm)
Limitations
- The retrospective study design limits causality.
- Lack of long-term follow-up data on the stability of clinical outcomes.
- The study may not have captured the full extent of healing because of the relatively short re-evaluation period (i.e., 2–6 months following subgingival instrumentation).
Conclusions & impact
- Age and disease severity are effective criteria for identifying patients who would benefit from adjunctive antibiotic therapy in periodontitis management.
- This approach can potentially limit unnecessary antibiotic prescriptions.
- Patients treated with antibiotics following the criteria of age and PPD (<56 years and PPD ≥5mm in ≥35% of sites) benefitted the most from the use of antibiotics.
- This study supports the use of age and clinical severity as criteria for systemicantibiotic delivery in periodontitis, potentially reducing over-prescription and aligning with public-health recommendations on antibiotics use.
Rapporteur: Michele Morandini, supervised by Prof. Giovanni E. Salvi
Affiliation: Postgraduate programme in periodontology, University of Bern, Switzerland
With kind permission from Wiley Online Library. Copyright © 1999-2024 John Wiley & Sons, Inc. All rights reserved