Issue No. 143
Summarized from Journal of Clinical Periodontology, Volume 52, Issue 11, November 2025, 1605-1615
Editor: James Deschner, chair, EFP scientific affairs committee
Which emergence profile is best for implant-supported crowns in the aesthetic zone?
Authors: Janina Endres, Franz J. Strauss, Marina Siegenthaler, Nadja Naenni, Ronald E. Jung, Daniel S. Thoma
Background
The design of a restoration on implants is crucial for guiding the transition from the implant platform to the mucosal margin, directly influencing peri-implant healing, tissue maturation, and early clinical outcomes. Most peri-implant tissue changes occur within the first year after loading, but the emergence profile continues to influence long-term aesthetics, mucosal dimensions, and overall tissue health beyond this period.
The shape of the peri-implant mucosa appears to depend strongly on the crown’s emergence profile. A concave emergence profile generally promotes better mucosal stability and facilitates prevention of mucosal recession, thereby preserving aesthetics. In contrast, convex profiles have been associated with complications such as mucosal recession and peri-implantitis.
The interim (12-month) analysis of the three-year clinical trial summarized here reported a higher frequency of mid-facial recessions after the use of crowns with convex emergence profile.1
While current evidence supports concave designs as the preferred option, convex profiles may still be indicated in specific anatomical situations, such as when the implant is positioned too far orally or near the marginal mucosa. Nevertheless, robust data on the intermediate-term performance of concave versus convex emergence profiles remain limited.
Aim
This three-year clinical trial aimed to assess the clinical, radiographic, and profilometric outcomes of implant-supported restorations with different emergence profiles, to determine whether aesthetic and clinical results deteriorate or remain stable over time.
Materials and methods
- Participants:
- Forty-seven patients each received a single dental implant (OsseoSpeed Tx, Astra Tech Implant System, Dentsply Sirona Implants) in the aesthetic zone of the maxilla or mandible, including premolars.
- Study design:
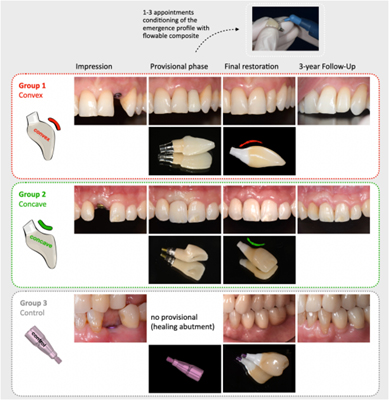
- Randomized controlled clinical trial with three groups:
- Concave (n = 16)
- Convex (n = 15)
- Control (n = 16; titanium healing abutment with a flat emergence profile)
- Randomization occurred three to four months after implant placement.
- Randomized controlled clinical trial with three groups:
- Provisional restorations:
- In test groups, under-contoured provisionals were adjusted using flowable composite to create concave or convex emergence profiles.
- Contours were refined weekly until symmetry with the contralateral tooth was achieved.
- Definitive restorations:
- Screw-retained monolithic zirconia crowns on individualized zirconia abutments reproducing the provisional emergence profile.
- Follow-up schedule:
- Baseline (seven to 10 days post-restoration, T0), and follow-ups at six (T1), 12 (T2), and 36 months (T3).
- Clinical and radiographic assessments:
- Primary outcome: mid-facial mucosal recession (mm).
- Secondary outcomes: modified Pink Esthetic Score (PES), probing depth (PD), bleeding on probing (BOP), plaque, buccal keratinized tissue (KT) width and thickness, and marginal bone level (MBL) on standardized radiographs.
- Mucosal changes analysed by profilometry of cast models.
- Peri-implant conditions diagnosed according to established classifications.
- Statistical analysis:
- Linear mixed-effects models assessed changes over time (fixed effects: treatment group, time, interaction; random effect: patient).
- Predictors of mid-facial recession analysed by multivariable logistic regression, adjusted for keratinized-tissue and soft-tissue thickness.
- Reliability tested using intraclass correlation coefficients (ICC).
- Significance level set at α = 0.05.
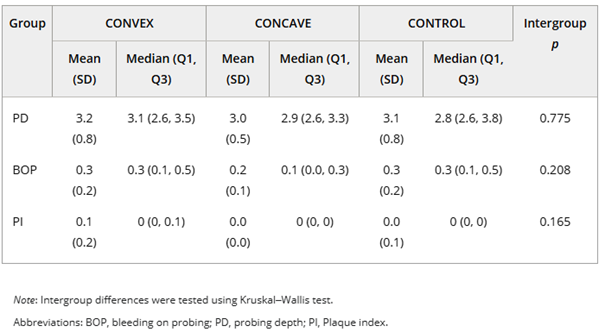
Note: Intergroup differences were tested using the Kruskal–Wallis test.
Abbreviations: BOP, bleeding on probing; PD, probing depth; PI, Plaque index.
Results
- A total of 42 patients completed the three-year re-examination.
- Mid-facial mucosal recession:
- Frequency at T2/T3:
- Convex: 64.3% / 46.7%
- Concave: 14.3% / 13.3%
- Control: 31.4% / 40%
- T2 comparisons:
- Convex vs. Concave: OR = 13.3 (95% CI 1.2–138.5, p = 0.030). Implants with convex emergence profile were about 13 times more likely to show mucosal recession: statistically significant.
- Control vs. Concave: OR = 3.3 (p = 0.335). No significant difference.
- Soft-tissue thickness and keratinized-tissue width: no significant effect.
- T3 comparisons:
- Convex vs. Concave: OR = 7.3 (95% CI 1.0–52.1, p = 0.048). Significantly higher risk of recession in the convex group after three years.
- Control vs. Concave: OR = 3.1 (p = 0.232). No significant difference.
- Soft-tissue thickness and keratinized-tissue width: no significant effect.
- Frequency at T2/T3:
- Mean mucosal level change (mm):
- Concave and control groups: negative (coronal) shifts at T3.
- Convex: 0.72 ± 0.60 (T2), 0.15 ± 1.10 (T3). Apical shifts decreased from T2 to T3.
- Indicates a coronal shift of the mucosal margin from T2 to T3 in all groups.
- Other clinical outcomes at T3: No significant intergroup differences in PD, BOP, plaque, peri-implant mucositis, PES, peri-implant tissue width, or MBL.
- Profilometric analysis: There were significant differences between groups in contour shape at region of interest 3 (ROI-3), but no difference in the magnitude of change.
Limitations
- The article provides no information on peri-implant or general maintenance of the patients during the three-year follow-up.
- Recession was measured as the apical shift of the mid-facial mucosa using a periodontal probe. However, many values fell within the instrument’s measurement margin of error, limiting precision.
- Some methodological details are missing, such as the type of periodontal probe used.
- No numerical threshold, range, or angle was defined to distinguish concave from convex emergence profiles.
- Patient-reported outcomes were not assessed.
- The transferability of these findings to posterior sites remains unclear and should be addressed in future studies.
- The clinical value of preparing the peri-implant mucosa with customized provisional screw-retained crowns may be questioned compared with crowns with a straight emergence profile placed after the use of a simple healing abutment.
Conclusions and impact
- Implants restored with a convex emergence profile showed a significantly higher risk of mid-facial mucosal recession, mainly within the first year after crown placement but also up to three years.
- Soft-tissue levels remained stable thereafter, suggesting that most peri-implant mucosal changes occur during the initial post-restorative period.
- A convex profile may limit soft-tissue maturation and restrict coronal migration (“creeping attachment”) during healing.
- BOP values were consistently lower in the concave group, although overall clinical parameters did not differ significantly between groups.
- The emergence profile defined during provisionalization exerts a lasting influence on the stability and health of peri-implant soft tissue.
Choosing a concave emergence profile during provisional and definitive crown design may limit mid-facial recession and promote soft-tissue stability, particularly in the first year, thereby enhancing long-term aesthetic outcomes in implant-supported restorations.
Footnote
1. Marina Siegenthaler, Franz J. Strauss, Felix Gamper, Christoph H. F. Hämmerle, Ronald E. Jung, and Daniel S. Thoma. 2022. “Anterior Implant Restorations With a Convex Emergence Profile Increase the Frequency of Recession: 12-Month Results of a Randomized Controlled Clinical Trial.” Journal of Clinical Periodontology 49: 1145–1157. https:// doi. org/ 10.1111/ jcpe. 13696).
Rapporteur: Patrizia Chiara Winkler supervised by Prof. Peter Eickholz (programme director)
Affiliation: Postgraduate programme in periodontology, Goethe University Frankfurt am Main, Germany
With kind permission from Wiley Online Library. Copyright © 1999-2025 John Wiley & Sons, Inc. All rights reserved