Publications Hub, EuroPerio, Treatment, Article
What are the limits for non-surgical peri-implantitis therapy?
12 May 2025
Peri-implantitis is a growing global problem. An interactive session at EuroPerio11 will focus on non-surgical procedures as a treatment option, covering sub-marginal instrumentation techniques and the use of systemic antibiotics and chemical decontaminants. Three cases will be presented and discussed, and the audience will then vote for the best procedure. Session moderator Antonio Liñares presents the issues and speakers Raluca Cosgarea, Ignacio Sanz Sánchez, and Ioannis Polyzois outline their non-surgical approaches.
Antonio Líñares: 'It is important to try to save the implant'
I think the most important part is that non-surgical and minimally invasive surgical procedures are now in fashion in medicine and dentistry. In fact, this can be extended to the current management of peri-implant diseases. Thus, you can get good results with a simple and minimally invasive approach.
I have been working in this field for the last 20 years and proposed this kind of protocol back then, when the consensus was that most of the time you needed to perform surgeries to treat peri-implantitis.
I started to develop a protocol based on the histopathological features of the lesion. Today, more and more colleagues are seeing that non-surgical therapies can be used very easily in a simple protocol.
Of course, an alternative therapy is to remove the implant. But if you do that, you will create a very deep bone defect. And to grow back bone vertically is really challenging. To me, it is important to try to save the implant, at least for some years, and to extend its life.
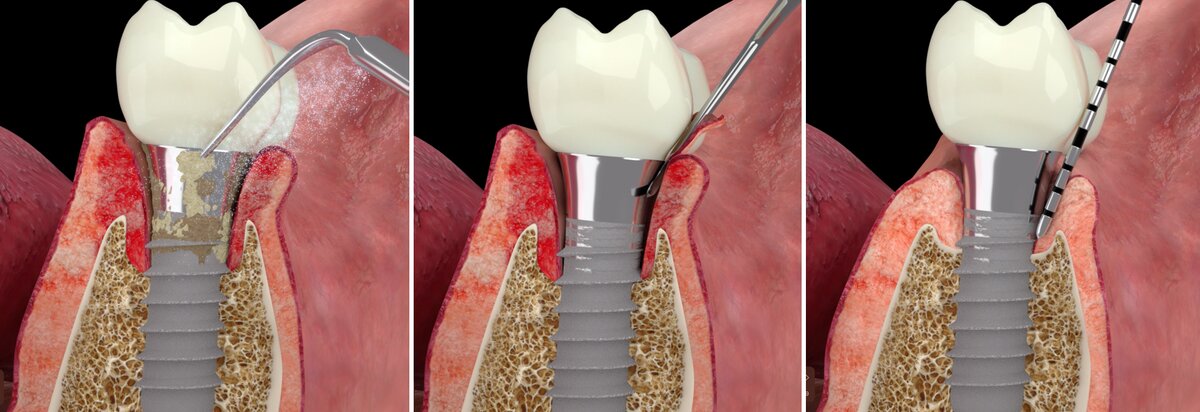
One of the key issues we face is how to treat this infection of the soft tissues surrounding the implant and how to decontaminate the implant surface. Remember that the implant—as a non-biological entity—gets contaminated rather than infected. Thus, in addition to sub-marginal instrumentation, we may have to use some adjunctive chemicals to reduce the infection of the soft tissues and the contamination of the implant.
This might include the use of specific systemic antibiotics. Of course, we are not going to give antibiotics to every single patient with peri-implantitis, but some patients will benefit more from them.
Raluca Cosgarea: 'We do not currently have any optimal or perfect tools'
Since peri-implantitis represents a complex plaque-associated pathological condition of the implant-supporting structures—often characterised by an unpredictable and accelerating pattern of disease progression—its treatment remains a big challenge for all clinicians.
Treatment aims at resolution of inflammation and arresting tissue loss. Effective biofilm removal and decontamination of the affected implant surfaces are prerequisites for achieving these goals.
At EuroPerio11, I will discuss different possibilities for mechanical/physical biofilm removal from implant surfaces, looking also at adjunctives including lasers and air-abrasive systems. Presenting the current data on this topic, I will highlight the efficacy and limitations of these methods.
On short-term basis, with most of the methods there is some improvement in clinical parameters. Some lasers have had a positive impact on inflammation reduction, but the evidence from high-quality studies is still scarce and data is contradictory because of the heterogeneity in the protocols used.
In terms of overcoming the mechanical limits, we do not currently have any optimal or perfect tools to access and remove non-surgically the entire biofilm from the contaminated implant surfaces. Thus, mechanical/physical decontamination in the non-surgical approach to peri-implantitis may be seen as a pre-step for the surgical treatment of advanced peri-implantitis lesions.
Ignacio Sanz Sánchez: 'We have successfully reduced surgery rates by around 90%'
It is important to acknowledge the limitations of conventional non-surgical and surgical treatment options for peri-implantitis. These options may not achieve optimal disease resolution, and there is a lack of consistency in patient-reported outcome measures and predictability.
Today, we are transitioning from a conventional non-surgical or conventional surgical approach to a new method that falls between the two. We have defined this as a minimally invasive flapless surgical approach.
The primary goal of minimally invasive approaches is to minimise the morbidity of clinical procedures. This is achieved by using techniques and instruments that reduce tissue trauma and maintain tissue architecture, benefit the healing phase, improve clinical results, increase visibility, and reduce treatment time. Furthermore, minimally invasive surgical and nonsurgical procedures enhance the biologic cellular principles underpinning regeneration and repair.
Today, we are proud to announce that, thanks to our innovative approach, we have successfully reduced surgery rates by around 90%. This treatment is non-surgical for the patient and does not involve the use of sutures or blades.
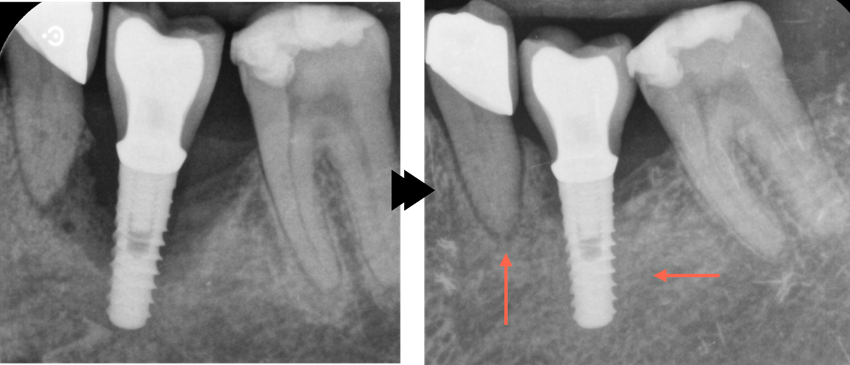
A study of more than 100 patients and almost 350 implants was conducted to assess the impact of systemic antibiotics, with a particular focus on Azithromycin, which can be administered in a single daily dose over a period of three days. Following a healing period of between one and five years, complete disease resolution was achieved in more than 54% of the implants, with 85% of them presenting probing depths of no more than five millimetres.
While the potential benefits of antibiotics are evident, the rise of antimicrobial resistances poses a significant public health concern, underscoring the urgent need to explore alternative solutions. At EuroPerio11, I will present the preliminary data on a new product that has shown promising results.
Ioannis Polyzois: 'The use of adjunctive chemical decontamination must be carefully considered'
A wide range of instruments and devices are currently available for sub-marginal instrumentation of implant surfaces affected by peri-implantitis. However, evidence does not support the clear superiority of any single method over others.
While adjunctive chemical decontamination may offer minimal additional benefits—such as slight improvements in bleeding on probing and pocket-depth reduction—its use must be carefully considered. The chosen chemical agents should not compromise the integrity or properties of the implant surface.
Healing following treatment has generally been more favourable around implants with machined surfaces. Nevertheless, the clinical relevance of this observation remains limited, given that most modern implants feature moderately rough surfaces specifically designed to enhance osseointegration. In certain high-risk patient populations, the use of hybrid implants may offer a viable alternative.
Effective non-surgical interventions must extend beyond the mere decontamination of the implant surface. A comprehensive therapeutic strategy should also address the peri-implant hard and soft tissues, aiming to facilitate bone regeneration and support the formation of a robust epithelial seal. In this context, platelet-rich fibrin (PRF) has demonstrated promising potential to enhance regenerative outcomes and reduce soft-tissue recession.
Additionally, resonance frequency analysis (RFA) serves as a valuable adjunctive tool for monitoring implant stability and the healing process, both in the immediate post-treatment phase and during long-term maintenance.
Ultimately, the long-term success and stability of peri-implantitis treatment hinge on strict adherence to individualized oral-hygiene protocols. Equally important is the identification and management of contributing factors related to the prosthetic supra-structure, as well as any local or systemic conditions that may have precipitated or exacerbated the disease process.
Biographies
Antonio Liñares is an assistant professor in periodontology at the University of Santiago de Compostela. Since 2007 he has been an honorary research fellow at the Eastman Dental Institute in London, and since 2016 an honorary clinical senior lecturer at the Queen Mary University of London. He owns a clinical practice dedicated to periodontology and implant dentistry in A Coruña (Spain). He was awarded the Fonseca Prize for research by the Spanish Society of Periodontology and Osseointegration in 2007 and ITI Schroeder Prize in preclinical research in 2017.
Raluca Cosgarea is an associate professor at the Clinic for Periodontology, Operative and Preventive Dentistry at the University of Bonn (Germany) and dean of studies for dentistry at the Medical Faculty, University of Bonn. Her research focuses on antimicrobial periodontal therapy, regenerative and mucogingival periodontal surgery, and the treatment of peri-implant infections. In 2022, she won the Jaccard-EFP Research Prize for a paper on the use of systemic antibiotics in patients with aggressive periodontitis.
Ignacio Sanz Sánchez has a degree in dentistry, master’s degree in dental science, and PhD from the Complutense University of Madrid, where he has been an associate professor of periodontics since 2017. He has a private practice in periodontics and implant dentistry and is a member of the SEPA Foundation.
Ioannis Polyzois is an associate professor and consultant in periodontology at the Dublin Dental University Hospital at Trinity College where he is currently the director of the EFP- and ICSTD-accredited postgraduate programme in periodontology. In June 2019 he took over the role of director of postgraduate teaching and learning. He is deputy chair of the EFP’s Scientific Affairs Committee.
Nonsurgical therapy for peri-implantitis: what are the limits? EuroPerio11 | Vienna | Thursday 15 May, 16.30-18.00
EuroPerio11 | Vienna | 14-17 May: Information and Registration




