![]()
2 April 2024
Economist Impact white paper sheds light on the burden of oral diseases in France
Categories:Institutional, Publications
In a recent Economist Impact white paper, commissioned by the EFP and supported by Haleon, the growing burden of caries and periodontitis, was highlighted, drawing attention to the need for concerted action by governments to reduce inequalities in oral health.
The report, focusing on the economic and health impacts of these diseases, calls for a shift towards a preventive approach, stresses the urgency of integrating oral health into the broader non-communicable diseases (NCDs) agenda. Oral diseases, having surpassed other NCDs in terms of global prevalence, are often neglected in mainstream health discussions, despite caries and severe periodontitis affecting about 2 billion and 1 billion people globally. The World Health Organization (WHO) has also recommended pivoting to a preventive approach for oral diseases and integrating oral care with NCDs care into the universal health care (UHC) agenda.
In France, the financial burden of caries on individuals and the healthcare system is substantial. The cost of caries for the French population aged 12-65 is estimated at 14.646 billion US$, with a lifetime cost per person of 21,036 US$. This burden is disproportionately heavier on the most deprived, with a cost per person reaching 25,850 US$.
The president of the French Society of Periodontology and Implantology (SFPIO), Doctor Caroline Fouque, reflecting on the findings, emphasised the importance of preventive measures. "The impact of oral diseases on overall health and the financial burden they impose cannot be overstated. There's an urgent need for increased awareness and prevention, which could significantly reduce healthcare costs and improve the quality of life," she stated.
Caries, a leading cause of hospitalisation among children in some high-income countries, accounts for 5-10% of healthcare budgets in these nations. This significant financial impact underscores the need for a shift in focus towards preventive care, which not only alleviates the burden on healthcare systems but also improves long-term health outcomes.
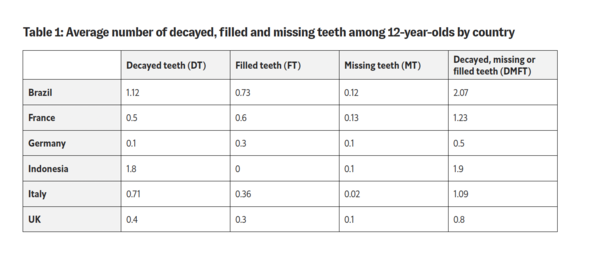
Despite France being one of the first European countries to introduce a tax on sweetened beverages the average number of decayed, filled and missing teeth among 12-year-olds is 1,23 - the highest among the developed countries included in the study. In 2018, the law was amended to introduce progressive taxation based on increasing sugar content rather than a flat tax rate. A survey showed that 65% of adults polled favoured the taxation scheme, with the number rising to 76% if the tax gains were reinvested into the healthcare system.
The report underlines the importance of comprehensive interventions in reducing caries-related direct costs. As well as sugar taxes, measures such as community water fluoridation (that currently does not exist in France) and improving access to quality fluoride toothpaste, can lead to significant reductions in treatment costs, particularly among the most deprived groups.
An interesting initiative in France is the Alliance for a Cavity-Free Future (ACFF) pilot for a new hybrid remuneration system for dentists. It’s focus is on improving access to quality care and better clinical outcomes, especially for marginalised communities. Over 600 dentists have been recruited to cover round 15000 people with over 6 million euros invested in the EXPRESO project. This initiative represents a model that could potentially be replicated and scaled in other countries. An external auditor will perform an economic evaluation of the system and a bespoke online system will be used to collect data.
Professor Nicola West, the EFP secretary general, called for robust data collection on the health burden and costs of oral health across Europe to inform policy decisions: "To effectively address the oral health crisis, we need comprehensive data on oral health conditions and their cost to society.” She added: “We also need more, and better, epidemiological studies and we must measure the effectiveness of preventive interventions. This data is crucial for guiding policy makers and ensuring universal access to dental care."
The white paper also emphasises the critical need for collaboration between medical and dental professionals. General practitioners (GPs) play a pivotal role as they are often the first point of contact for patients. By incorporating oral health checks into routine medical examinations, GPs can identify potential oral health issues early and refer patients to dental professionals for specialized care. Medical students should also be made aware of the interconnection between oral health and overall health.
The current dental care model in France is limited due to the absence of dental hygienists in the formal dental workforce. Dental hygienists, along with other allied dental care professionals like dental therapists, are crucial for expanding preventive care and managing oral health more effectively. Their role in providing routine dental care, educating patients about oral hygiene, and assisting in preventive treatments is vital. Integrating these professionals into the dental team can fill existing gaps, especially in preventive services, and can help dentists manage their workload more efficiently.
The white paper’s findings present a compelling case for prioritising oral health and preventive care. By integrating oral care within broader healthcare, a more effective approach to health and well-being can be achieved. The need for increased awareness, better data collection, and the implementation of preventive strategies is clear, as is the call for governments and health organisations to take decisive action in this regard.